Healthcare Payer Technology and Services Market Size, Share & Trends Analysis Report by Component (Software Solutions, Services), Deployment Mode, Payer Type, Organization Size, Service Model, Pricing Model, Integration Level, End-Users, and Geography (North America, Europe, Asia Pacific, Middle East, Africa, and South America) – Global Industry Data, Trends, and Forecasts, 2025–2035
|
|
|
Segmental Data Insights |
|
|
Demand Trends |
|
|
Competitive Landscape |
|
|
Strategic Development |
|
|
Future Outlook & Opportunities |
|
Healthcare Payer Technology and Services Market Size, Share, and Growth
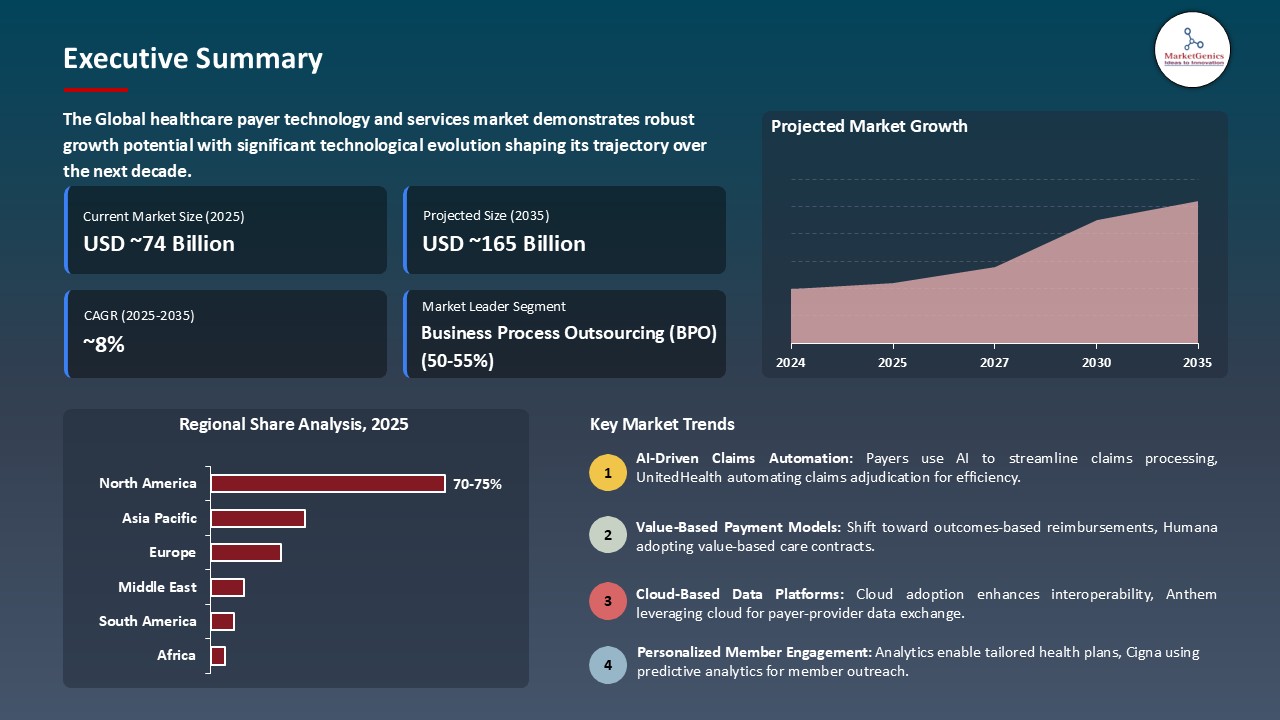
The global healthcare payer technology and services market is witnessing strong growth, valued at USD 73.6 billion in 2025 and projected to reach USD 164.9 billion by 2035, expanding at a CAGR of 8.4% during the forecast period. North America leads the healthcare payer technology and services market due to strong healthcare infrastructure, high adoption of digital health technologies, and supportive regulatory frameworks such as FDA approvals.
Venkat Kavarthapu, EVP of operations at Edifecs said that, “By embedding intelligent agents directly into our Population Payment Management platform, we’re helping our customers scale programs faster, cut costs, and improve performance. This marks a shift from theoretical AI to practical solutions that understand the nuances of value-based contracts while processing healthcare data securely, at scale, and in compliance with industry standards”.
The regulatory pressures including Centers for Medicare & Medicaid Services (CMS) interoperability regulations and international data-sharing frameworks forcing payers to switch to advanced technology platforms that would provide secure data transfer, real-time analytic solutions, and clear communication among healthcare ecosystems necessitating modernization and expansion in the healthcare payer technology and services sector. As an example, in March 2025 Availity introduced its Payer-to-Payer Data Exchange program through the Connectivity Hub to comply with CMS interoperability and prior authorization requirements and facilitate the smooth exchange of data between payers via API.
The healthcare payer technology and services market is growing through strategic partnerships and alliances between payers, providers, and technology vendors, which allow the realization of data interoperability, increase the pace of value-based care, develop automation, analytics, and digital engagement solutions. An example that illustrates this is in 2025, athenahealth, Humana and Your Health collaborated to incorporate real-time payer-provider data transmission, lessening the administrative load and bridging the care gap during the point of care- advancing interoperability.
The healthcare payer technology and services market is witnessing significant opportunities as a result of increased regulatory requirements of smooth data sharing and interoperability. With interoperability and modernization of prior-authorization processes being enforced by CMS, as well as ONC, payers are putting funds in APIs based, FHIR-enabled, and cloud-native solutions. This would allow safe real-time data sharing, enhance the experience of members, efficiency of claims, and collaboration between payers and providers and increase transparency and compliance. As an example, Humana and Providence recently established a FHIR-based data exchange partnership (In October 2025) to support the real-time payer-provider interoperability, improving care coordination and value-based care provision.
Healthcare Payer Technology and Services Market Dynamics and Trends
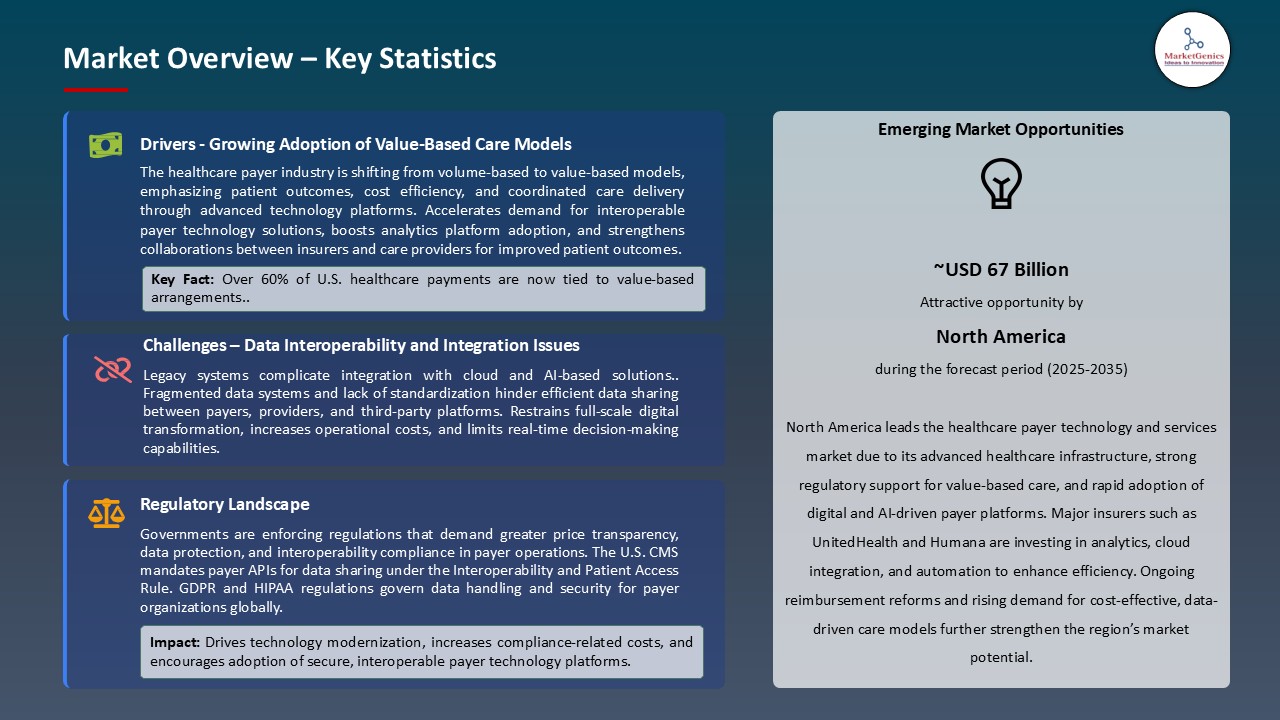
Driver: Value-Based Care Contracts Require Advanced Analytics and Care Management Platforms
- A significant force behind the healthcare payer technology and services Market is the increasing use of value-based care (VBC) contracts, with payers moving away of fee-based systems towards outcomes-based reimbursement practices. These contracts require an integrated system of data, predictive analytics, and population health management to assess the performance of the provider, monitor patient outcomes, and make risk-adjusted payments.
- The AI-based Population Payment Management Platform was launched by Edifecs in 2025, to facilitate value-based payment (VBP) contract management to payers. The solution uses advanced analytics and automation to handle risk-based agreements, track performance in the provider, and streamline reimbursement results to show the increasing use of smart platforms to facilitate value-based care processes.
- The development enhances the level of payer digital transformation through the improvement of data-driven decision-making, the efficiency of the contract, and the strengthening of the market transition to value-based and outcomes-oriented models of healthcare.
Restraint: Legacy System Modernization Complexity Delays Technology Transformation
- The healthcare payer technology and services market is under a lot of pressure because of the intricacy of the legacy IT systems that most payers continue to use in claims processing, managing members and data storage. These old infrastructures tend not to be interoperable, scalable, and with integration features necessary to operate advanced analytic, cloud deployment, and value-based care.
- As a process that requires several stages, is resource intensive, and involves a large amount of data migration, reconfiguring workflows, and aligning them with regulatory requirements such as the HIPAA and CMS interoperability requirements. Loss of service, data integrity and excessive cost of implementation are also threats to payers that tend to discourage quick transformation efforts.
- Slow digital transformation, slow innovation is also due to the inability to break free of legacy systems, which in turn is a barrier to payer competitiveness and overall development and modernization of the healthcare payer technology and services market.
Opportunity: Medicare Advantage Growth Drives Technology Investment in Senior-Focused Capabilities
- The healthcare payer technology and services market has a high growth potential due to the rapid growth of Medicare Advantage (MA) programs, with payers moving quickly to invest in senior-centric digital platforms, advanced analytics, and care coordination tools, ensuring the management of aging populations, better outcomes, and increased efficiency of value-based reimbursement.
- Wellcare also declared its intention to launch Medicare Advantage and Medicare Prescription Drug Plan in 2025 to more than 51 million members across the country, a move that shows the increased growth of the elderly market. This action highlights the increased availability of opportunities to payers to invest in highly digitalized platforms, analytics, and engagement solutions to improve the management of senior care, which spurs technology investment in healthcare payer technology and services market.
- The growth will drive the increasing investment of payers on senior-focused digital infrastructure and drive innovation and market development in the healthcare payer technology and services market.
Key Trend: Artificial Intelligence Automates Administrative Functions and Enhances Decision-Making
- Artificial Intelligence (AI) is quickly revolutionizing the Healthcare Payer Technology and Services Market by automating multifaceted administrative processes and allowing data-driven decision making in payer activities. Claims, authorizations, fraud, and member engagement are being automated with AI which is cutting down on the manual work and expenses, and machine learning and NLP provide real time insights which improve risk assessment, care management and policy decisions.
- HealthEdge, under Bain Capital, merged with UST HealthProof in 2025, to develop the AI-native HealthEdge Payer Intelligence Platform, which is the unification of claims, payments, and member engagement through intelligent automation and analytics as a significant step in AI-based administrative efficiencies, strategic choices, and digital transformation in the healthcare payer technology and services market.
- The development of AI will enhance the speed of intelligent automation and data-driven processes, increase the efficiency of payers, their agility, and their overall competitiveness in the market.
Healthcare-Payer-Technology-and-Services-Market Analysis and Segmental Data
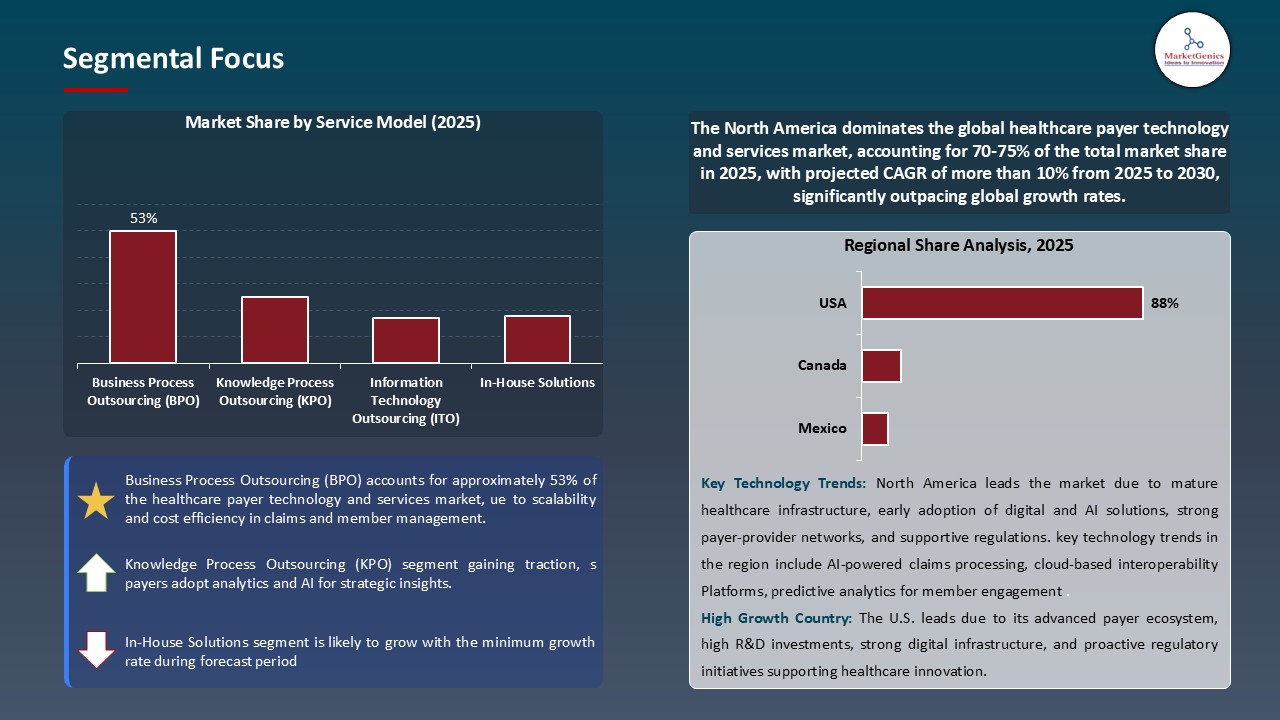
Business Process Outsourcing (BPO) Dominate Global Healthcare Payer Technology and Services Market
- The business process outsourcing segment leads the payer technology and services market worldwide, due to the increasing demands of the payers to improve administrative processes, cut operational expenses, and enhance service delivery. BPO companies provide highly qualified skills in claims processing, billing, member enrollment, and revenue cycle management that enable healthcare payers to concentrate efforts on strategic programs like digital transformation and value care.
- For instance, in 2025, under its Business Process as a Service (BPaaS) Power offer, a major U.S. health payer engaged Firstsource Solutions Ltd to improve claims management and make its offerings more responsive to its members. The partnership makes use of AI-powered automation and analytics to simplify administrative processes to allow the payer to concentrate on the well-being and value care of its members.
- The automation, AI, and analytics implementation in the outsourced operations can also be used to increase accuracy, compliance, and scalability, which makes BPO even stronger on the market.
North America Leads Global Healthcare Payer Technology and Services Market Demand
- North America dominates the healthcare payer technology and services market globally, with a high healthcare expenditure, a well-developed payer ecosystem, and well-developed technological integration of both administrative and member management systems. The emphasis of the region in digital transformation, regulatory development, and collaboration with IT and BPO vendors is still compelling efficient and innovative development.
- Optum introduced its program in 2025 to transform the claims and reimbursement model to help remove complexity and waste in administration in payer operations. Optum facilitates the improvement to transparency of payers and providers by integrating advanced analytics, automation and interoperable data platforms to ensure swift reimbursement cycles. This project is an indication of the fact that the U.S. market is highly concentrated on digital transformation and efficiency of its operations, which strengthens the leadership of the North American region.
- Additionally, the existence of major industry participants, with the early implementation of data-driven and interoperable solutions, only enhances the dominance of North America in market trends globally.
Healthcare-Payer-Technology-and-Services-Market Ecosystem
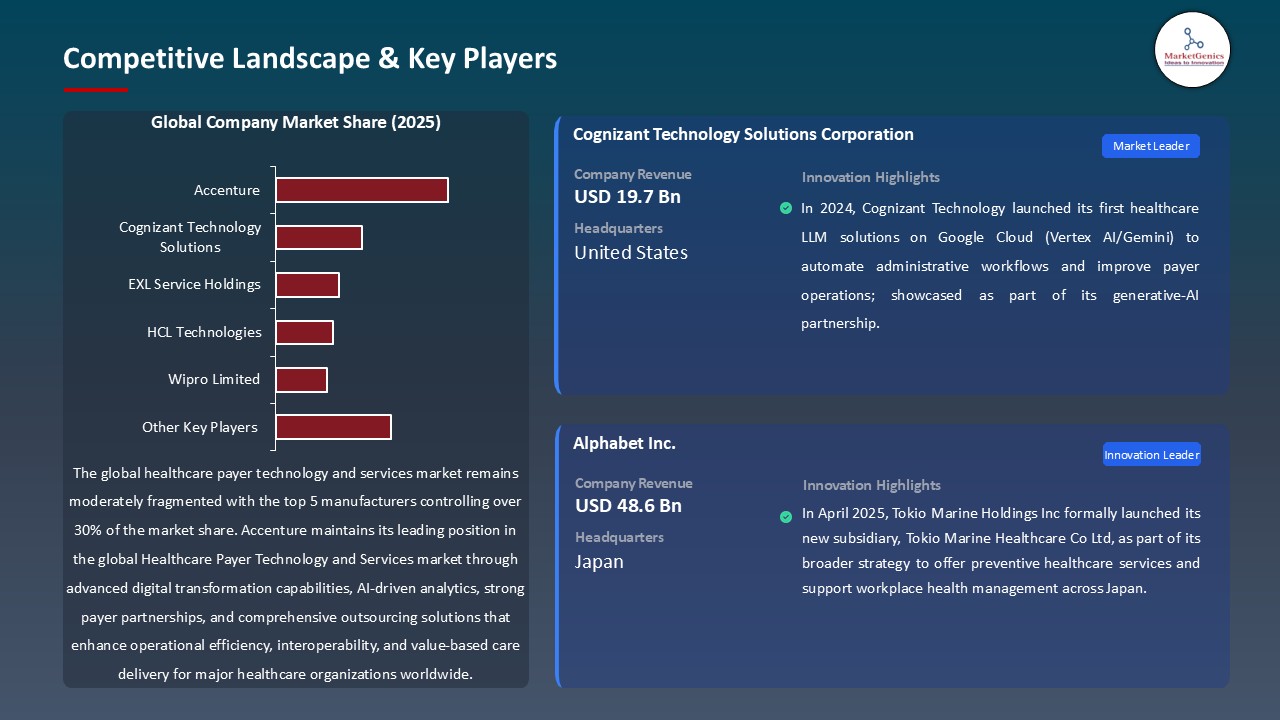
The global healthcare payer technologies and services market is moderately fragmented with major market participants including Accenture, Cognizant Technology Solutions, EXL Service holdings, HCL technologies and Wipro limited holding relatively 32 percent of the market. Such businesses are on the forefront in terms of innovation offering end-to-end payer technology solutions, business process outsourcing (BPO), automation, analytics, and digital transformation services. The high level of domain knowledge, their own proprietary platforms, and the experience of long-lasting collaboration with large insurance providers allow them to manage claims better, comply with regulations, and engage with members.
Additionally, technology integrators and service providers are critical in assisting payers to have scalable IT infrastructure, migration to the cloud and process optimization that relies on AI. To illustrate, Cognizant uses its TriZetto Healthcare Products and payer-oriented digital platforms to transform the fundamental operations and enhance administrative efficiency. Such strategic capabilities and technological improvements create a significant obstacle to new entrants and solidify the position of the established players in the international healthcare payer technology and services sector.
Recent Development and Strategic Overview:
-
In September 2025, Oracle Health introduced an AI-powered payer–provider collaboration suite to accelerate value-based care adoption by automating authorizations, eligibility, and claims processing. Integrating advanced analytics and real-time data sharing, the platform enhances interoperability, transparency, and care coordination—advancing intelligent automation within the healthcare payer technology and services Market.
- In March 2025, PointClickCare launched its “Transitions of Care” solution, offering real-time, EHR-agnostic admission and discharge data insights to help Medicare Advantage plans improve post-discharge coordination, reduce readmissions, and boost CMS Star Ratings—strengthening data-driven care continuity and payer performance in the healthcare payer technology and services market.
Report Scope
|
Detail |
|
|
Market Size in 2025 |
USD 73.6 Bn |
|
Market Forecast Value in 2035 |
USD 164.9 Bn |
|
Growth Rate (CAGR) |
8.4% |
|
Forecast Period |
2025 – 2035 |
|
Historical Data Available for |
2021 – 2024 |
|
Market Size Units |
US$ Billion for Value |
|
Report Format |
Electronic (PDF) + Excel |
|
North America |
Europe |
Asia Pacific |
Middle East |
Africa |
South America |
|
|
|
|
|
|
|
Companies Covered |
|||||
|
|
|
|
|
|
Healthcare-Payer-Technology-and-Services-Market Segmentation and Highlights
|
Segment |
Sub-segment |
|
Healthcare Payer Technology and Services Market, By Component |
|
|
Healthcare Payer Technology and Services Market, By Deployment Mode |
|
|
Healthcare Payer Technology and Services Market, By Payer Type |
|
|
Healthcare Payer Technology and Services Market, By Organization Size |
|
|
Healthcare Payer Technology and Services Market, By Service Model |
|
|
Healthcare Payer Technology and Services Market, By Pricing Model |
|
|
Healthcare Payer Technology and Services Market, By Integration Level |
|
|
Healthcare Payer Technology and Services Market, By End-users |
|
Frequently Asked Questions
The global healthcare payer technology and services market was valued at USD 73.6 Bn in 2025
The global healthcare payer technology and services market is expected to grow at a CAGR of 8.4% from 2025 to 2035
The key factors driving demand for the healthcare payer technology and services market include rising healthcare costs, regulatory compliance needs, digital transformation initiatives, and growing adoption of automation and analytics to enhance efficiency and member experience
In terms of service model, the business process outsourcing segment accounted for the major share in 2025.
North America is the most attractive region for healthcare payer technology and services market
Prominent players operating in the global healthcare payer technology and services market are Accenture, Allscripts Healthcare Solutions, Atos SE, CGI Inc., Cognizant Technology Solutions, Conduent Inc., Conifer Health Solutions, DXC Technology, Evolent Health, EXL Service Holdings, Genpact, HCL Technologies, Hinduja Global Solutions (HGS), IBM Corporation, Infosys, Inovalon Holdings, NTT DATA Corporation, Tata Consultancy Services (TCS), TriZetto Corporation, UnitedHealth Group (Optum), Wipro Limited, and other Key Players
Table of Contents
- 1. Research Methodology and Assumptions
- 1.1. Definitions
- 1.2. Research Design and Approach
- 1.3. Data Collection Methods
- 1.4. Base Estimates and Calculations
- 1.5. Forecasting Models
- 1.5.1. Key Forecast Factors & Impact Analysis
- 1.6. Secondary Research
- 1.6.1. Open Sources
- 1.6.2. Paid Databases
- 1.6.3. Associations
- 1.7. Primary Research
- 1.7.1. Primary Sources
- 1.7.2. Primary Interviews with Stakeholders across Ecosystem
- 2. Executive Summary
- 2.1. Global Healthcare Payer Technology and Services Market Outlook
- 2.1.1. Healthcare Payer Technology and Services Market Size (Value - US$ Bn), and Forecasts, 2021-2035
- 2.1.2. Compounded Annual Growth Rate Analysis
- 2.1.3. Growth Opportunity Analysis
- 2.1.4. Segmental Share Analysis
- 2.1.5. Geographical Share Analysis
- 2.2. Market Analysis and Facts
- 2.3. Supply-Demand Analysis
- 2.4. Competitive Benchmarking
- 2.5. Go-to- Market Strategy
- 2.5.1. Customer/ End-use Industry Assessment
- 2.5.2. Growth Opportunity Data, 2025-2035
- 2.5.2.1. Regional Data
- 2.5.2.2. Country Data
- 2.5.2.3. Segmental Data
- 2.5.3. Identification of Potential Market Spaces
- 2.5.4. GAP Analysis
- 2.5.5. Potential Attractive Price Points
- 2.5.6. Prevailing Market Risks & Challenges
- 2.5.7. Preferred Sales & Marketing Strategies
- 2.5.8. Key Recommendations and Analysis
- 2.5.9. A Way Forward
- 2.1. Global Healthcare Payer Technology and Services Market Outlook
- 3. Industry Data and Premium Insights
- 3.1. Global Healthcare & Pharmaceutical Industry Overview, 2025
- 3.1.1. Healthcare & Pharmaceutical Industry Ecosystem Analysis
- 3.1.2. Key Trends for Healthcare & Pharmaceutical Industry
- 3.1.3. Regional Distribution for Healthcare & Pharmaceutical Industry
- 3.2. Supplier Customer Data
- 3.3. Technology Roadmap and Developments
- 3.4. Trade Analysis
- 3.4.1. Import & Export Analysis, 2025
- 3.4.2. Top Importing Countries
- 3.4.3. Top Exporting Countries
- 3.5. Trump Tariff Impact Analysis
- 3.5.1. Manufacturer
- 3.5.1.1. Based on the component & Raw material
- 3.5.2. Supply Chain
- 3.5.3. End Consumer
- 3.5.1. Manufacturer
- 3.6. Raw Material Analysis
- 3.1. Global Healthcare & Pharmaceutical Industry Overview, 2025
- 4. Market Overview
- 4.1. Market Dynamics
- 4.1.1. Drivers
- 4.1.1.1. Value-based care & cost-containment pressures driving payer tech adoption
- 4.1.1.2. Advanced analytics/AI for risk stratification, personalization, and fraud detection
- 4.1.1.3. Regulatory mandates and interoperability pushing digital modernization
- 4.1.2. Restraints
- 4.1.2.1. Data privacy, security, and integration challenges
- 4.1.2.2. High implementation costs and legacy-system inertia
- 4.1.1. Drivers
- 4.2. Key Trend Analysis
- 4.3. Regulatory Framework
- 4.3.1. Key Regulations, Norms, and Subsidies, by Key Countries
- 4.3.2. Tariffs and Standards
- 4.3.3. Impact Analysis of Regulations on the Market
- 4.4. Value Chain Analysis
- 4.5. Porter’s Five Forces Analysis
- 4.6. PESTEL Analysis
- 4.7. Global Healthcare Payer Technology and Services Market Demand
- 4.7.1. Historical Market Size - in Value (US$ Bn), 2020-2024
- 4.7.2. Current and Future Market Size - in Value (US$ Bn), 2025–2035
- 4.7.2.1. Y-o-Y Growth Trends
- 4.7.2.2. Absolute $ Opportunity Assessment
- 4.1. Market Dynamics
- 5. Competition Landscape
- 5.1. Competition structure
- 5.1.1. Fragmented v/s consolidated
- 5.2. Company Share Analysis, 2025
- 5.2.1. Global Company Market Share
- 5.2.2. By Region
- 5.2.2.1. North America
- 5.2.2.2. Europe
- 5.2.2.3. Asia Pacific
- 5.2.2.4. Middle East
- 5.2.2.5. Africa
- 5.2.2.6. South America
- 5.3. Product Comparison Matrix
- 5.3.1. Specifications
- 5.3.2. Market Positioning
- 5.3.3. Pricing
- 5.1. Competition structure
- 6. Global Healthcare Payer Technology and Services Market Analysis, By Component
- 6.1. Key Segment Analysis
- 6.2. Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, By Component, 2021-2035
- 6.2.1. Software Solutions
- 6.2.1.1. Claims Management Software
- 6.2.1.2. Provider Network Management Software
- 6.2.1.3. Payment Integrity Software
- 6.2.1.4. Care Management Software
- 6.2.1.5. Member Management Software
- 6.2.1.6. Fraud, Waste, and Abuse Detection Software
- 6.2.1.7. Analytics and Reporting Software
- 6.2.1.8. Others
- 6.2.2. Services
- 6.2.2.1. Implementation Services
- 6.2.2.2. Consulting Services
- 6.2.2.3. Training and Education Services
- 6.2.2.4. Support and Maintenance Services
- 6.2.2.5. Managed Services
- 6.2.2.6. Others
- 6.2.1. Software Solutions
- 7. Global Healthcare Payer Technology and Services Market Analysis, By Deployment Mode
- 7.1. Key Segment Analysis
- 7.2. Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, By Deployment Mode, 2021-2035
- 7.2.1. On-Premises
- 7.2.2. Cloud-Based
- 7.2.3. Hosted Solutions
- 8. Global Healthcare Payer Technology and Services Market Analysis and Forecasts,By Payer Type
- 8.1. Key Findings
- 8.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Payer Type, 2021-2035
- 8.2.1. Private Payers
- 8.2.1.1. Commercial Health Insurance Companies
- 8.2.1.2. Managed Care Organizations (MCOs)
- 8.2.1.3. Third-Party Administrators (TPAs)
- 8.2.1.4. Others
- 8.2.2. Public Payers
- 8.2.2.1. Medicare Programs
- 8.2.2.2. Medicaid Programs
- 8.2.2.3. Government Health Agencies
- 8.2.2.4. Others
- 8.2.3. Hybrid Payers
- 8.2.1. Private Payers
- 9. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Organization Size
- 9.1. Key Findings
- 9.2. Healthcare Payer Technology and Services Market Size (Vo Value - US$ Mn), Analysis, and Forecasts, By Organization Size, 2021-2035
- 9.2.1. Large Enterprises
- 9.2.2. Small and Medium-sized Enterprises (SMEs)
- 10. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Service Model
- 10.1. Key Findings
- 10.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Service Model, 2021-2035
- 10.2.1. Business Process Outsourcing (BPO)
- 10.2.2. Knowledge Process Outsourcing (KPO)
- 10.2.3. Information Technology Outsourcing (ITO)
- 10.2.4. In-House Solutions
- 11. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Pricing Model
- 11.1. Key Findings
- 11.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Pricing Model, 2021-2035
- 11.2.1. Subscription-Based
- 11.2.2. Perpetual License
- 11.2.3. Pay-Per-Use
- 11.2.4. Transaction-Based
- 12. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Integration Level
- 12.1. Key Findings
- 12.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Integration Level, 2021-2035
- 12.2.1. Standalone Solutions
- 12.2.2. Integrated Platforms
- 12.2.3. Enterprise-Wide Systems
- 12.2.4. Interoperable Systems
- 13. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By End-users
- 13.1. Key Findings
- 13.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By End-users, 2021-2035
- 13.2.1. Health Insurance Companies
- 13.2.1.1. Member Enrollment and Eligibility Verification
- 13.2.1.2. Premium Billing and Collection
- 13.2.1.3. Claims Adjudication and Processing
- 13.2.1.4. Provider Credentialing and Network Management
- 13.2.1.5. Utilization Management
- 13.2.1.6. Risk Assessment and Underwriting
- 13.2.1.7. Customer Service and Support
- 13.2.1.8. Fraud Detection and Prevention
- 13.2.1.9. Others
- 13.2.2. Managed Care Organizations (MCOs)
- 13.2.2.1. Care Coordination and Management
- 13.2.2.2. Disease Management Programs
- 13.2.2.3. Population Health Management
- 13.2.2.4. Member Engagement Platforms
- 13.2.2.5. Pharmacy Benefit Management
- 13.2.2.6. Value-Based Care Analytics
- 13.2.2.7. Others
- 13.2.3. Third-Party Administrators (TPAs)
- 13.2.3.1. Claims Processing and Administration
- 13.2.3.2. Benefits Administration
- 13.2.3.3. COBRA Administration
- 13.2.3.4. Health Savings Account (HSA) Management
- 13.2.3.5. Flexible Spending Account (FSA) Administration
- 13.2.3.6. Provider Payment Processing
- 13.2.3.7. Others
- 13.2.4. Government Health Programs
- 13.2.4.1. Medicare/Medicaid Claims Processing
- 13.2.4.2. Eligibility Determination Systems
- 13.2.4.3. Program Integrity and Audit
- 13.2.4.4. Appeals and Grievance Management
- 13.2.4.5. Public Health Reporting
- 13.2.4.6. Others
- 13.2.5. Self-Insured Employers
- 13.2.5.1. Employee Benefits Administration
- 13.2.5.2. Health Plan Management
- 13.2.5.3. Wellness Program Management
- 13.2.5.4. Claims Analytics and Reporting
- 13.2.5.5. Cost Containment Strategies
- 13.2.5.6. Employee Health Data Analytics
- 13.2.5.7. Others
- 13.2.6. Pharmacy Benefit Managers (PBMs)
- 13.2.7. Healthcare Provider Organizations
- 13.2.8. Health and Wellness Companies
- 13.2.9. Other End-users
- 13.2.1. Health Insurance Companies
- 14. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, by Region
- 14.1. Key Findings
- 14.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, by Region, 2021-2035
- 14.2.1. North America
- 14.2.2. Europe
- 14.2.3. Asia Pacific
- 14.2.4. Middle East
- 14.2.5. Africa
- 14.2.6. South America
- 15. North America Healthcare Payer Technology and Services Market Analysis
- 15.1. Key Segment Analysis
- 15.2. Regional Snapshot
- 15.3. North America Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 15.3.1. Component
- 15.3.2. Deployment Mode
- 15.3.3. Payer Type
- 15.3.4. Organization Size
- 15.3.5. Service Model
- 15.3.6. Pricing Model
- 15.3.7. Integration Level
- 15.3.8. End-Users
- 15.3.9. Country
- 15.3.9.1. USA
- 15.3.9.2. Canada
- 15.3.9.3. Mexico
- 15.4. USA Healthcare Payer Technology and Services Market
- 15.4.1. Country Segmental Analysis
- 15.4.2. Component
- 15.4.3. Deployment Mode
- 15.4.4. Payer Type
- 15.4.5. Organization Size
- 15.4.6. Service Model
- 15.4.7. Pricing Model
- 15.4.8. Integration Level
- 15.4.9. End-Users
- 15.5. Canada Healthcare Payer Technology and Services Market
- 15.5.1. Country Segmental Analysis
- 15.5.2. Component
- 15.5.3. Deployment Mode
- 15.5.4. Payer Type
- 15.5.5. Organization Size
- 15.5.6. Service Model
- 15.5.7. Pricing Model
- 15.5.8. Integration Level
- 15.5.9. End-Users
- 15.6. Mexico Healthcare Payer Technology and Services Market
- 15.6.1. Country Segmental Analysis
- 15.6.2. Component
- 15.6.3. Deployment Mode
- 15.6.4. Payer Type
- 15.6.5. Organization Size
- 15.6.6. Service Model
- 15.6.7. Pricing Model
- 15.6.8. Integration Level
- 15.6.9. End-Users
- 16. Europe Healthcare Payer Technology and Services Market Analysis
- 16.1. Key Segment Analysis
- 16.2. Regional Snapshot
- 16.3. Europe Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 16.3.1. Component
- 16.3.2. Deployment Mode
- 16.3.3. Payer Type
- 16.3.4. Organization Size
- 16.3.5. Service Model
- 16.3.6. Pricing Model
- 16.3.7. Integration Level
- 16.3.8. End-Users
- 16.3.9. Country
- 16.3.9.1. Germany
- 16.3.9.2. United Kingdom
- 16.3.9.3. France
- 16.3.9.4. Italy
- 16.3.9.5. Spain
- 16.3.9.6. Netherlands
- 16.3.9.7. Nordic Countries
- 16.3.9.8. Poland
- 16.3.9.9. Russia & CIS
- 16.3.9.10. Rest of Europe
- 16.4. Germany Healthcare Payer Technology and Services Market
- 16.4.1. Country Segmental Analysis
- 16.4.2. Component
- 16.4.3. Deployment Mode
- 16.4.4. Payer Type
- 16.4.5. Organization Size
- 16.4.6. Service Model
- 16.4.7. Pricing Model
- 16.4.8. Integration Level
- 16.4.9. End-Users
- 16.5. United Kingdom Healthcare Payer Technology and Services Market
- 16.5.1. Country Segmental Analysis
- 16.5.2. Component
- 16.5.3. Deployment Mode
- 16.5.4. Payer Type
- 16.5.5. Organization Size
- 16.5.6. Service Model
- 16.5.7. Pricing Model
- 16.5.8. Integration Level
- 16.5.9. End-Users
- 16.6. France Healthcare Payer Technology and Services Market
- 16.6.1. Country Segmental Analysis
- 16.6.2. Component
- 16.6.3. Deployment Mode
- 16.6.4. Payer Type
- 16.6.5. Organization Size
- 16.6.6. Service Model
- 16.6.7. Pricing Model
- 16.6.8. Integration Level
- 16.6.9. End-Users
- 16.7. Italy Healthcare Payer Technology and Services Market
- 16.7.1. Country Segmental Analysis
- 16.7.2. Component
- 16.7.3. Deployment Mode
- 16.7.4. Payer Type
- 16.7.5. Organization Size
- 16.7.6. Service Model
- 16.7.7. Pricing Model
- 16.7.8. Integration Level
- 16.7.9. End-Users
- 16.8. Spain Healthcare Payer Technology and Services Market
- 16.8.1. Component
- 16.8.2. Deployment Mode
- 16.8.3. Payer Type
- 16.8.4. Organization Size
- 16.8.5. Service Model
- 16.8.6. Pricing Model
- 16.8.7. Integration Level
- 16.8.8. End-Users
- 16.9. Netherlands Healthcare Payer Technology and Services Market
- 16.9.1. Country Segmental Analysis
- 16.9.2. Component
- 16.9.3. Deployment Mode
- 16.9.4. Payer Type
- 16.9.5. Organization Size
- 16.9.6. Service Model
- 16.9.7. Pricing Model
- 16.9.8. Integration Level
- 16.9.9. End-Users
- 16.10. Nordic Countries Healthcare Payer Technology and Services Market
- 16.10.1. Country Segmental Analysis
- 16.10.2. Component
- 16.10.3. Deployment Mode
- 16.10.4. Payer Type
- 16.10.5. Organization Size
- 16.10.6. Service Model
- 16.10.7. Pricing Model
- 16.10.8. Integration Level
- 16.10.9. End-Users
- 16.11. Poland Healthcare Payer Technology and Services Market
- 16.11.1. Country Segmental Analysis
- 16.11.2. Component
- 16.11.3. Deployment Mode
- 16.11.4. Payer Type
- 16.11.5. Organization Size
- 16.11.6. Service Model
- 16.11.7. Pricing Model
- 16.11.8. Integration Level
- 16.11.9. End-Users
- 16.12. Russia & CIS Healthcare Payer Technology and Services Market
- 16.12.1. Country Segmental Analysis
- 16.12.2. Component
- 16.12.3. Deployment Mode
- 16.12.4. Payer Type
- 16.12.5. Organization Size
- 16.12.6. Service Model
- 16.12.7. Pricing Model
- 16.12.8. Integration Level
- 16.12.9. End-Users
- 16.13. Rest of Europe Healthcare Payer Technology and Services Market
- 16.13.1. Country Segmental Analysis
- 16.13.2. Component
- 16.13.3. Deployment Mode
- 16.13.4. Payer Type
- 16.13.5. Organization Size
- 16.13.6. Service Model
- 16.13.7. Pricing Model
- 16.13.8. Integration Level
- 16.13.9. End-Users
- 17. Asia Pacific Healthcare Payer Technology and Services Market Analysis
- 17.1. Key Segment Analysis
- 17.2. Regional Snapshot
- 17.3. East Asia Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 17.3.1. Component
- 17.3.2. Deployment Mode
- 17.3.3. Payer Type
- 17.3.4. Organization Size
- 17.3.5. Service Model
- 17.3.6. Pricing Model
- 17.3.7. Integration Level
- 17.3.8. End-Users
- 17.3.9. Country
- 17.3.9.1. China
- 17.3.9.2. India
- 17.3.9.3. Japan
- 17.3.9.4. South Korea
- 17.3.9.5. Australia and New Zealand
- 17.3.9.6. Indonesia
- 17.3.9.7. Malaysia
- 17.3.9.8. Thailand
- 17.3.9.9. Vietnam
- 17.3.9.10. Rest of Asia Pacific
- 17.4. China Healthcare Payer Technology and Services Market
- 17.4.1. Country Segmental Analysis
- 17.4.2. Component
- 17.4.3. Deployment Mode
- 17.4.4. Payer Type
- 17.4.5. Organization Size
- 17.4.6. Service Model
- 17.4.7. Pricing Model
- 17.4.8. Integration Level
- 17.4.9. End-Users
- 17.5. India Healthcare Payer Technology and Services Market
- 17.5.1. Country Segmental Analysis
- 17.5.2. Component
- 17.5.3. Deployment Mode
- 17.5.4. Payer Type
- 17.5.5. Organization Size
- 17.5.6. Service Model
- 17.5.7. Pricing Model
- 17.5.8. Integration Level
- 17.5.9. End-Users
- 17.6. Japan Healthcare Payer Technology and Services Market
- 17.6.1. Country Segmental Analysis
- 17.6.2. Component
- 17.6.3. Deployment Mode
- 17.6.4. Payer Type
- 17.6.5. Organization Size
- 17.6.6. Service Model
- 17.6.7. Pricing Model
- 17.6.8. Integration Level
- 17.6.9. End-Users
- 17.7. South Korea Healthcare Payer Technology and Services Market
- 17.7.1. Country Segmental Analysis
- 17.7.2. Component
- 17.7.3. Deployment Mode
- 17.7.4. Payer Type
- 17.7.5. Organization Size
- 17.7.6. Service Model
- 17.7.7. Pricing Model
- 17.7.8. Integration Level
- 17.7.9. End-Users
- 17.8. Australia and New Zealand Healthcare Payer Technology and Services Market
- 17.8.1. Country Segmental Analysis
- 17.8.2. Component
- 17.8.3. Deployment Mode
- 17.8.4. Payer Type
- 17.8.5. Organization Size
- 17.8.6. Service Model
- 17.8.7. Pricing Model
- 17.8.8. Integration Level
- 17.8.9. End-Users
- 17.9. Indonesia Healthcare Payer Technology and Services Market
- 17.9.1. Country Segmental Analysis
- 17.9.2. Component
- 17.9.3. Deployment Mode
- 17.9.4. Payer Type
- 17.9.5. Organization Size
- 17.9.6. Service Model
- 17.9.7. Pricing Model
- 17.9.8. Integration Level
- 17.9.9. End-Users
- 17.10. Malaysia Healthcare Payer Technology and Services Market
- 17.10.1. Country Segmental Analysis
- 17.10.2. Component
- 17.10.3. Deployment Mode
- 17.10.4. Payer Type
- 17.10.5. Organization Size
- 17.10.6. Service Model
- 17.10.7. Pricing Model
- 17.10.8. Integration Level
- 17.10.9. End-Users
- 17.11. Thailand Healthcare Payer Technology and Services Market
- 17.11.1. Country Segmental Analysis
- 17.11.2. Component
- 17.11.3. Deployment Mode
- 17.11.4. Payer Type
- 17.11.5. Organization Size
- 17.11.6. Service Model
- 17.11.7. Pricing Model
- 17.11.8. Integration Level
- 17.11.9. End-Users
- 17.12. Vietnam Healthcare Payer Technology and Services Market
- 17.12.1. Country Segmental Analysis
- 17.12.2. Component
- 17.12.3. Deployment Mode
- 17.12.4. Payer Type
- 17.12.5. Organization Size
- 17.12.6. Service Model
- 17.12.7. Pricing Model
- 17.12.8. Integration Level
- 17.12.9. End-Users
- 17.13. Rest of Asia Pacific Healthcare Payer Technology and Services Market
- 17.13.1. Country Segmental Analysis
- 17.13.2. Component
- 17.13.3. Deployment Mode
- 17.13.4. Payer Type
- 17.13.5. Organization Size
- 17.13.6. Service Model
- 17.13.7. Pricing Model
- 17.13.8. Integration Level
- 17.13.9. End-Users
- 18. Middle East Healthcare Payer Technology and Services Market Analysis
- 18.1. Key Segment Analysis
- 18.2. Regional Snapshot
- 18.3. Middle East Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 18.3.1. Component
- 18.3.2. Deployment Mode
- 18.3.3. Payer Type
- 18.3.4. Organization Size
- 18.3.5. Service Model
- 18.3.6. Pricing Model
- 18.3.7. Integration Level
- 18.3.8. End-Users
- 18.3.9. Country
- 18.3.9.1. Turkey
- 18.3.9.2. UAE
- 18.3.9.3. Saudi Arabia
- 18.3.9.4. Israel
- 18.3.9.5. Rest of Middle East
- 18.4. Turkey Healthcare Payer Technology and Services Market
- 18.4.1. Country Segmental Analysis
- 18.4.2. Component
- 18.4.3. Deployment Mode
- 18.4.4. Payer Type
- 18.4.5. Organization Size
- 18.4.6. Service Model
- 18.4.7. Pricing Model
- 18.4.8. Integration Level
- 18.4.9. End-Users
- 18.5. UAE Healthcare Payer Technology and Services Market
- 18.5.1. Country Segmental Analysis
- 18.5.2. Component
- 18.5.3. Deployment Mode
- 18.5.4. Payer Type
- 18.5.5. Organization Size
- 18.5.6. Service Model
- 18.5.7. Pricing Model
- 18.5.8. Integration Level
- 18.5.9. End-Users
- 18.6. Saudi Arabia Healthcare Payer Technology and Services Market
- 18.6.1. Country Segmental Analysis
- 18.6.2. Component
- 18.6.3. Deployment Mode
- 18.6.4. Payer Type
- 18.6.5. Organization Size
- 18.6.6. Service Model
- 18.6.7. Pricing Model
- 18.6.8. Integration Level
- 18.6.9. End-Users
- 18.7. Israel Healthcare Payer Technology and Services Market
- 18.7.1. Country Segmental Analysis
- 18.7.2. Component
- 18.7.3. Deployment Mode
- 18.7.4. Payer Type
- 18.7.5. Organization Size
- 18.7.6. Service Model
- 18.7.7. Pricing Model
- 18.7.8. Integration Level
- 18.7.9. End-Users
- 18.8. Rest of Middle East Healthcare Payer Technology and Services Market
- 18.8.1. Country Segmental Analysis
- 18.8.2. Component
- 18.8.3. Deployment Mode
- 18.8.4. Payer Type
- 18.8.5. Organization Size
- 18.8.6. Service Model
- 18.8.7. Pricing Model
- 18.8.8. Integration Level
- 18.8.9. End-Users
- 19. Africa Healthcare Payer Technology and Services Market Analysis
- 19.1. Key Segment Analysis
- 19.2. Regional Snapshot
- 19.3. Africa Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 19.3.1. Component
- 19.3.2. Deployment Mode
- 19.3.3. Payer Type
- 19.3.4. Organization Size
- 19.3.5. Service Model
- 19.3.6. Pricing Model
- 19.3.7. Integration Level
- 19.3.8. End-Users
- 19.3.9. Country
- 19.3.9.1. South Africa
- 19.3.9.2. Egypt
- 19.3.9.3. Nigeria
- 19.3.9.4. Algeria
- 19.3.9.5. Rest of Africa
- 19.4. South Africa Healthcare Payer Technology and Services Market
- 19.4.1. Country Segmental Analysis
- 19.4.2. Component
- 19.4.3. Deployment Mode
- 19.4.4. Payer Type
- 19.4.5. Organization Size
- 19.4.6. Service Model
- 19.4.7. Pricing Model
- 19.4.8. Integration Level
- 19.4.9. End-Users
- 19.5. Egypt Healthcare Payer Technology and Services Market
- 19.5.1. Country Segmental Analysis
- 19.5.2. Component
- 19.5.3. Deployment Mode
- 19.5.4. Payer Type
- 19.5.5. Organization Size
- 19.5.6. Service Model
- 19.5.7. Pricing Model
- 19.5.8. Integration Level
- 19.5.9. End-Users
- 19.6. Nigeria Healthcare Payer Technology and Services Market
- 19.6.1. Country Segmental Analysis
- 19.6.2. Component
- 19.6.3. Deployment Mode
- 19.6.4. Payer Type
- 19.6.5. Organization Size
- 19.6.6. Service Model
- 19.6.7. Pricing Model
- 19.6.8. Integration Level
- 19.6.9. End-Users
- 19.7. Algeria Healthcare Payer Technology and Services Market
- 19.7.1. Country Segmental Analysis
- 19.7.2. Component
- 19.7.3. Deployment Mode
- 19.7.4. Payer Type
- 19.7.5. Organization Size
- 19.7.6. Service Model
- 19.7.7. Pricing Model
- 19.7.8. Integration Level
- 19.7.9. End-Users
- 19.8. Rest of Africa Healthcare Payer Technology and Services Market
- 19.8.1. Country Segmental Analysis
- 19.8.2. Component
- 19.8.3. Deployment Mode
- 19.8.4. Payer Type
- 19.8.5. Organization Size
- 19.8.6. Service Model
- 19.8.7. Pricing Model
- 19.8.8. Integration Level
- 19.8.9. End-Users
- 20. South America Healthcare Payer Technology and Services Market Analysis
- 20.1. Key Segment Analysis
- 20.2. Regional Snapshot
- 20.3. Central and South Africa Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 20.3.1. Component
- 20.3.2. Deployment Mode
- 20.3.3. Payer Type
- 20.3.4. Organization Size
- 20.3.5. Service Model
- 20.3.6. Pricing Model
- 20.3.7. Integration Level
- 20.3.8. End-Users
- 20.3.9. Country
- 20.3.9.1. Brazil
- 20.3.9.2. Argentina
- 20.3.9.3. Rest of South America
- 20.4. Brazil Healthcare Payer Technology and Services Market
- 20.4.1. Country Segmental Analysis
- 20.4.2. Component
- 20.4.3. Deployment Mode
- 20.4.4. Payer Type
- 20.4.5. Organization Size
- 20.4.6. Service Model
- 20.4.7. Pricing Model
- 20.4.8. Integration Level
- 20.4.9. End-Users
- 20.5. Argentina Healthcare Payer Technology and Services Market
- 20.5.1. Country Segmental Analysis
- 20.5.2. Component
- 20.5.3. Deployment Mode
- 20.5.4. Payer Type
- 20.5.5. Organization Size
- 20.5.6. Service Model
- 20.5.7. Pricing Model
- 20.5.8. Integration Level
- 20.5.9. End-Users
- 20.6. Rest of South America Healthcare Payer Technology and Services Market
- 20.6.1. Country Segmental Analysis
- 20.6.2. Component
- 20.6.3. Deployment Mode
- 20.6.4. Payer Type
- 20.6.5. Organization Size
- 20.6.6. Service Model
- 20.6.7. Pricing Model
- 20.6.8. Integration Level
- 20.6.9. End-Users
- 21. Key Players/ Company Profile
- 21.1. Accenture
- 21.1.1. Company Details/ Overview
- 21.1.2. Company Financials
- 21.1.3. Key Customers and Competitors
- 21.1.4. Business/ Industry Portfolio
- 21.1.5. Product Portfolio/ Specification Details
- 21.1.6. Pricing Data
- 21.1.7. Strategic Overview
- 21.1.8. Recent Developments
- 21.2. Allscripts Healthcare Solutions
- 21.3. Atos SE
- 21.4. CGI Inc.
- 21.5. Cognizant Technology Solutions
- 21.6. Conduent Inc.
- 21.7. Conifer Health Solutions
- 21.8. DXC Technology
- 21.9. Evolent Health
- 21.10. EXL Service Holdings
- 21.11. Genpact
- 21.12. HCL Technologies
- 21.13. Hinduja Global Solutions (HGS)
- 21.14. IBM Corporation
- 21.15. Infosys
- 21.16. Inovalon Holdings
- 21.17. NTT DATA Corporation
- 21.18. Tata Consultancy Services (TCS)
- 21.19. TriZetto Corporation
- 21.20. UnitedHealth Group (Optum)
- 21.21. Wipro Limited
- 21.22. Other Key Players
- 21.1. Accenture
Note* - This is just tentative list of players. While providing the report, we will cover more number of players based on their revenue and share for each geography
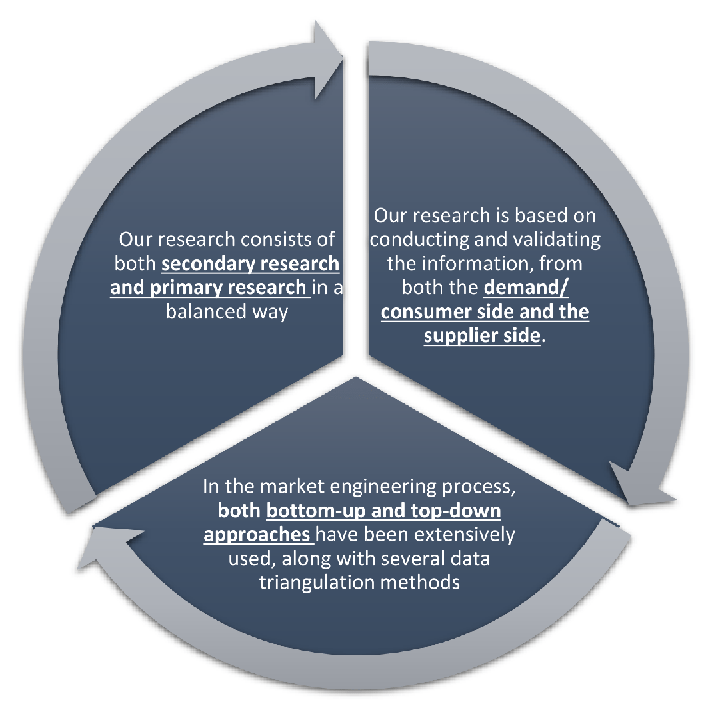
Our research design integrates both demand-side and supply-side analysis through a balanced combination of primary and secondary research methodologies. By utilizing both bottom-up and top-down approaches alongside rigorous data triangulation methods, we deliver robust market intelligence that supports strategic decision-making.
MarketGenics' comprehensive research design framework ensures the delivery of accurate, reliable, and actionable market intelligence. Through the integration of multiple research approaches, rigorous validation processes, and expert analysis, we provide our clients with the insights needed to make informed strategic decisions and capitalize on market opportunities.
MarketGenics leverages a dedicated industry panel of experts and a comprehensive suite of paid databases to effectively collect, consolidate, and analyze market intelligence.
Our approach has consistently proven to be reliable and effective in generating accurate market insights, identifying key industry trends, and uncovering emerging business opportunities.
Through both primary and secondary research, we capture and analyze critical company-level data such as manufacturing footprints, including technical centers, R&D facilities, sales offices, and headquarters.
Our expert panel further enhances our ability to estimate market size for specific brands based on validated field-level intelligence.
Our data mining techniques incorporate both parametric and non-parametric methods, allowing for structured data collection, sorting, processing, and cleaning.
Demand projections are derived from large-scale data sets analyzed through proprietary algorithms, culminating in robust and reliable market sizing.
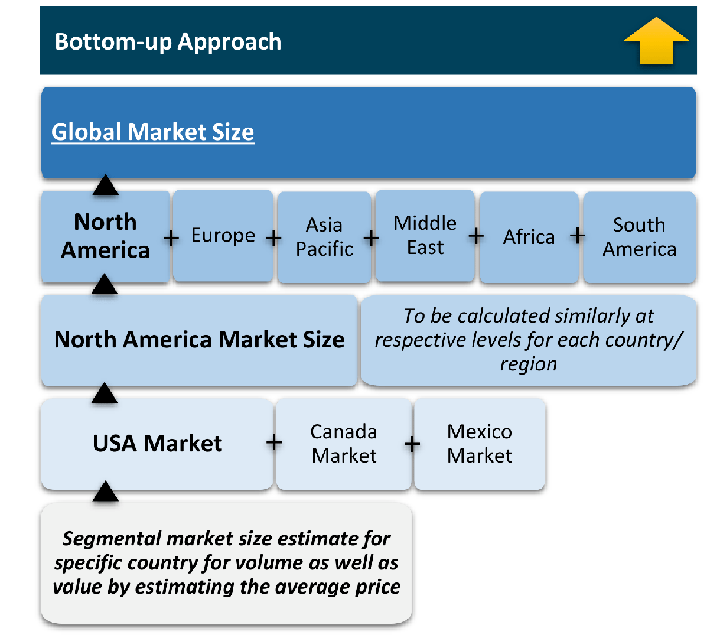
The bottom-up approach builds market estimates by starting with the smallest addressable market units and systematically aggregating them to create comprehensive market size projections.
This method begins with specific, granular data points and builds upward to create the complete market landscape.
Customer Analysis → Segmental Analysis → Geographical Analysis
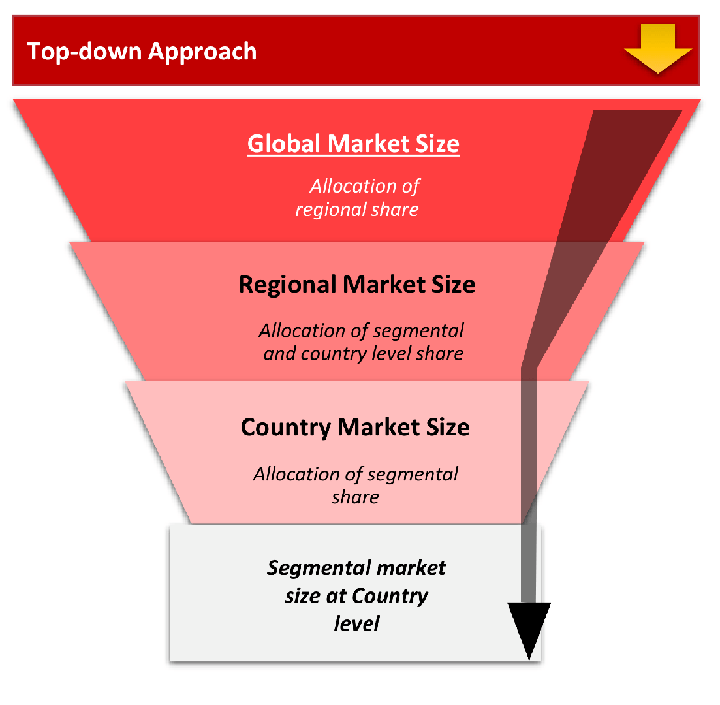
The top-down approach starts with the broadest possible market data and systematically narrows it down through a series of filters and assumptions to arrive at specific market segments or opportunities.
This method begins with the big picture and works downward to increasingly specific market slices.
TAM → SAM → SOM
While analysing the market, we extensively study secondary sources, directories, and databases to identify and collect information useful for this technical, market-oriented, and commercial report. Secondary sources that we utilize are not only the public sources, but it is combination of Open Source, Associations, Paid Databases, MG Repository & Knowledgebase and Others.
- Company websites, annual reports, financial reports, broker reports, and investor presentations
- National government documents, statistical databases and reports
- News articles, press releases and web-casts specific to the companies operating in the market, Magazines, reports, and others
- We gather information from commercial data sources for deriving company specific data such as segmental revenue, share for geography, product revenue, and others
- Internal and external proprietary databases (industry-specific), relevant patent, and regulatory databases
- Governing Bodies, Government Organizations
- Relevant Authorities, Country-specific Associations for Industries
We also employ the model mapping approach to estimate the product level market data through the players product portfolio
Primary research/ interviews is vital in analyzing the market. Most of the cases involves paid primary interviews. Primary sources includes primary interviews through e-mail interactions, telephonic interviews, surveys as well as face-to-face interviews with the different stakeholders across the value chain including several industry experts.
| Type of Respondents | Number of Primaries |
|---|---|
| Tier 2/3 Suppliers | ~20 |
| Tier 1 Suppliers | ~25 |
| End-users | ~25 |
| Industry Expert/ Panel/ Consultant | ~30 |
| Total | ~100 |
MG Knowledgebase
• Repository of industry blog, newsletter and case studies
• Online platform covering detailed market reports, and company profiles
- Historical Trends – Past market patterns, cycles, and major events that shaped how markets behave over time. Understanding past trends helps predict future behavior.
- Industry Factors – Specific characteristics of the industry like structure, regulations, and innovation cycles that affect market dynamics.
- Macroeconomic Factors – Economic conditions like GDP growth, inflation, and employment rates that affect how much money people have to spend.
- Demographic Factors – Population characteristics like age, income, and location that determine who can buy your product.
- Technology Factors – How quickly people adopt new technology and how much technology infrastructure exists.
- Regulatory Factors – Government rules, laws, and policies that can help or restrict market growth.
- Competitive Factors – Analyzing competition structure such as degree of competition and bargaining power of buyers and suppliers.
Multiple Regression Analysis
- Identify and quantify factors that drive market changes
- Statistical modeling to establish relationships between market drivers and outcomes
Time Series Analysis – Seasonal Patterns
- Understand regular cyclical patterns in market demand
- Advanced statistical techniques to separate trend, seasonal, and irregular components
Time Series Analysis – Trend Analysis
- Identify underlying market growth patterns and momentum
- Statistical analysis of historical data to project future trends
Expert Opinion – Expert Interviews
- Gather deep industry insights and contextual understanding
- In-depth interviews with key industry stakeholders
Multi-Scenario Development
- Prepare for uncertainty by modeling different possible futures
- Creating optimistic, pessimistic, and most likely scenarios
Time Series Analysis – Moving Averages
- Sophisticated forecasting for complex time series data
- Auto-regressive integrated moving average models with seasonal components
Econometric Models
- Apply economic theory to market forecasting
- Sophisticated economic models that account for market interactions
Expert Opinion – Delphi Method
- Harness collective wisdom of industry experts
- Structured, multi-round expert consultation process
Monte Carlo Simulation
- Quantify uncertainty and probability distributions
- Thousands of simulations with varying input parameters
Our research framework is built upon the fundamental principle of validating market intelligence from both demand and supply perspectives. This dual-sided approach ensures comprehensive market understanding and reduces the risk of single-source bias.
Demand-Side Analysis: We understand end-user/application behavior, preferences, and market needs along with the penetration of the product for specific application.
Supply-Side Analysis: We estimate overall market revenue, analyze the segmental share along with industry capacity, competitive landscape, and market structure.
Data triangulation is a validation technique that uses multiple methods, sources, or perspectives to examine the same research question, thereby increasing the credibility and reliability of research findings. In market research, triangulation serves as a quality assurance mechanism that helps identify and minimize bias, validate assumptions, and ensure accuracy in market estimates.
- Data Source Triangulation – Using multiple data sources to examine the same phenomenon
- Methodological Triangulation – Using multiple research methods to study the same research question
- Investigator Triangulation – Using multiple researchers or analysts to examine the same data
- Theoretical Triangulation – Using multiple theoretical perspectives to interpret the same data