A significant study discovering the market avenues on, “Healthcare Payer Technology and Services Market Size, Share & Trends Analysis Report by Component (Software Solutions, Services), Deployment Mode, Payer Type, Organization Size, Service Model, Pricing Model, Integration Level, End-Users, and Geography (North America, Europe, Asia Pacific, Middle East, Africa, and South America) – Global Industry Data, Trends, and Forecasts, 2025–2035” A holistic view of the market pathways in the healthcare payer technology and services market underscores revenue acceleration through three key levers scalable product line extensions, high‑maturity strategic partnerships
Global Healthcare Payer Technology and Services Market Forecast 2035:
According to the report, the global healthcare payer technology and services market is projected to expand from USD 73.6 billion in 2025 to USD 164.9 billion by 2035, registering a CAGR of 8.4%, the highest during the forecast period. The global market of Healthcare Payer Technology and Services is experiencing a rapid change in the usage of advanced digital technologies and outsourced services by the insurance providers to improve their ability to provide advanced services to the customers, adhere to the regulations, and ensure efficiency of their operations. The expansion of the market is substantially motivated by the necessity to simplify the administrative procedures, including claims management, enrollment, billing, and member engagement employing automation, artificial intelligence, and data analytics. Payers are using technology to enhance their population health data, facilitate value-based reimbursement patterns, and cut expenses linked to manual processes and fraud identification.
Additionally, the increasing emphasis on interoperability and cloud-based systems is allowing increasingly integrated, flexible and scalable payer ecosystems. Services providers that provide business process outsourcing, analytics-based decision support, and consulting services are also on the rise because the payers are also seeking specialized knowledge and flexibility. Nonetheless, issues like privacy of data, old IT infrastructure or sophisticated regulatory climate keep impeding smooth adoption. All in all, the market is moving towards digitally enabled data-driven payer operations, which focus on maximizing cost, member satisfaction, and value creation in the long term.
“Key Driver, Restraint, and Growth Opportunity Shaping the Global Healthcare Payer Technology and Services Market”
The escalating cost of healthcare is driving payers to embrace cost-optimization and efficiency-oriented technologies at a rising rate in order to remain profitable and provide affordable coverage. Payers organizations are experiencing financial strain due to administrative waste, amplifying claims volume, and escalating the cost of chronic disease treatment. In response, payers are spending on automation systems, AI-based claims adjudication, fraud prediction analytics, and cloud-based systems that simplify the work processes and minimize manual errors. These technologies do not only reduce administrative overhead but also enhance accuracy, reduce the processing time and decision making.
The lack of skilled professionals possessing knowledge in healthcare data analytics, regulatory compliance, and integration with IT systems is a significant constraint to the global Healthcare Payer Technology and Services market. The advanced payer technologies like AI-enabled claims processing, predictive analytics, and interoperable data platforms are difficult to implement and manage without a specialized knowledge that is unavailable to many organizations. The short supply of talent that can facilitate the healthcare operations with the complex digital tools gives way to delays in deployment, inefficient use of systems and dependency on outside vendors. This skill short does not only increase operational expenses but also reduces innovation and slows digital transformation of the payer ecosystem.
One of the most promising opportunities in the global healthcare payer technology and services market is the increasing use of cloud-based and interoperable solutions to provide real-time data exchange in all parts of the healthcare ecosystem. Cloud technologies enable payers to safely handle vast amounts of health and claims information, increase the scale ability, and cut down infrastructure expenses. As an example, in 2025, Edifecs released its Healthcare Interoperability Cloud, which is a SaaS platform allowing real-time data-sharing between 300+ payer clients using FHIR, EDI, and HL7 standards to meet the CMS-9115-F and 0057-F requirements, advancing the integration of the cloud-based interoperability and value-based care.
Regional Analysis of Global Healthcare Payer Technology and Services Market
- Healthcare payer technology and services market in North America is likely to be the most promising one due to well-developed digital health infrastructure, early automation and cloud-based payer platform adoption, and favorable regulatory changes that would promote interoperability and data-informed decisions. The region is dominated by the United States, which is motivated by its developed insurance ecosystem, investments by the CMS in value-based care initiatives, and the massive modernization of payer programs. Canada follows suit, whereby increasing investments in health IT and national approaches to digital health are improving payer efficiency and cross systems data integration. As an example, In June 2025, Inovaare Corporation was listed as a Sample Vendor again in the Gartner Hype Cycle of U.S. Healthcare Payers, 2025, due to its healthcare compliance and automation of operations.
- The Asia Pacific region is expected to experience the largest growth in the healthcare payer technology and services market because of the increasing healthcare digitalization, growing insurance coverage, and government-sponsored health reform programs that foster efficiency and transparency in payer operations. India, China, and Japan are among the countries that are driving this rise with such initiatives as nationwide digitization of health insurance, AI-based claims management, and acceptance of cloud-based health data systems that are accelerating the modernization of payer infrastructure and increasing the growth speed of the region.
Prominent players operating in the global healthcare payer technology and services market are Accenture, Allscripts Healthcare Solutions, Atos SE, CGI Inc., Cognizant Technology Solutions, Conduent Inc., Conifer Health Solutions, DXC Technology, Evolent Health, EXL Service Holdings, Genpact, HCL Technologies, Hinduja Global Solutions (HGS), IBM Corporation, Infosys, Inovalon Holdings, NTT DATA Corporation, Tata Consultancy Services (TCS), TriZetto Corporation, UnitedHealth Group (Optum), Wipro Limited, and other Key Players.
The global healthcare payer technology and services market has been segmented as follows:
Global Healthcare Payer Technology and Services Market Analysis, By Component
- Software Solutions
- Claims Management Software
- Provider Network Management Software
- Payment Integrity Software
- Care Management Software
- Member Management Software
- Fraud, Waste, and Abuse Detection Software
- Analytics and Reporting Software
- Others
- Services
- Implementation Services
- Consulting Services
- Training and Education Services
- Support and Maintenance Services
- Managed Services
- Others
Global Healthcare Payer Technology and Services Market Analysis, By Deployment Mode
- On-Premises
- Cloud-Based
- Hosted Solutions
Global Healthcare Payer Technology and Services Market Analysis, By Payer Type
- Private Payers
- Commercial Health Insurance Companies
- Managed Care Organizations (MCOs)
- Third-Party Administrators (TPAs)
- Others
- Public Payers
- Medicare Programs
- Medicaid Programs
- Government Health Agencies
- Others
- Hybrid Payers
Global Healthcare Payer Technology and Services Market Analysis, By Organization Size
- Large Enterprises
- Small and Medium-sized Enterprises (SMEs)
Global Healthcare Payer Technology and Services Market Analysis, By Service Model
- Business Process Outsourcing (BPO)
- Knowledge Process Outsourcing (KPO)
- Information Technology Outsourcing (ITO)
- In-House Solutions
Global Healthcare Payer Technology and Services Market Analysis, By Pricing Model
- Subscription-Based
- Perpetual License
- Pay-Per-Use
- Transaction-Based
Global Healthcare Payer Technology and Services Market Analysis, By Integration Level
- Standalone Solutions
- Integrated Platforms
- Enterprise-Wide Systems
- Interoperable Systems
Global Healthcare Payer Technology and Services Market Analysis, by End Users
- Health Insurance Companies
- Member Enrollment and Eligibility Verification
- Premium Billing and Collection
- Claims Adjudication and Processing
- Provider Credentialing and Network Management
- Utilization Management
- Risk Assessment and Underwriting
- Customer Service and Support
- Fraud Detection and Prevention
- Others
- Managed Care Organizations (MCOs)
- Care Coordination and Management
- Disease Management Programs
- Population Health Management
- Member Engagement Platforms
- Pharmacy Benefit Management
- Value-Based Care Analytics
- Others
- Third-Party Administrators (TPAs)
- Claims Processing and Administration
- Benefits Administration
- COBRA Administration
- Health Savings Account (HSA) Management
- Flexible Spending Account (FSA) Administration
- Provider Payment Processing
- Others
- Government Health Programs
- Medicare/Medicaid Claims Processing
- Eligibility Determination Systems
- Program Integrity and Audit
- Appeals and Grievance Management
- Public Health Reporting
- Others
- Self-Insured Employers
- Employee Benefits Administration
- Health Plan Management
- Wellness Program Management
- Claims Analytics and Reporting
- Cost Containment Strategies
- Employee Health Data Analytics
- Others
- Pharmacy Benefit Managers (PBMs)
- Healthcare Provider Organizations
- Health and Wellness Companies
- Other End-users
Global Healthcare Payer Technology and Services Market Analysis, By Region
About Us
MarketGenics is a global market research and management consulting company empowering decision makers from startups, Fortune 500 companies, non-profit organizations, universities and government institutions. Our main goal is to assist and partner organizations to make lasting strategic improvements and realize growth targets. Our industry research reports are designed to provide granular quantitative information, combined with key industry insights, aimed at assisting sustainable organizational development.
We serve clients on every aspect of strategy, including product development, application modeling, exploring new markets and tapping into niche growth opportunities.
Contact Us
USA Address:
800 N King Street Suite 304 #4208 Wilmington, DE 19801 United States.
+1(302)303-2617
info@marketgenics.co
India Address:
3rd floor, Indeco Equinox, Baner Road, Baner, Pune, Maharashtra 411045 India.
sales@marketgenics.co
Table of Contents
- 1. Research Methodology and Assumptions
- 1.1. Definitions
- 1.2. Research Design and Approach
- 1.3. Data Collection Methods
- 1.4. Base Estimates and Calculations
- 1.5. Forecasting Models
- 1.5.1. Key Forecast Factors & Impact Analysis
- 1.6. Secondary Research
- 1.6.1. Open Sources
- 1.6.2. Paid Databases
- 1.6.3. Associations
- 1.7. Primary Research
- 1.7.1. Primary Sources
- 1.7.2. Primary Interviews with Stakeholders across Ecosystem
- 2. Executive Summary
- 2.1. Global Healthcare Payer Technology and Services Market Outlook
- 2.1.1. Healthcare Payer Technology and Services Market Size (Value - US$ Bn), and Forecasts, 2021-2035
- 2.1.2. Compounded Annual Growth Rate Analysis
- 2.1.3. Growth Opportunity Analysis
- 2.1.4. Segmental Share Analysis
- 2.1.5. Geographical Share Analysis
- 2.2. Market Analysis and Facts
- 2.3. Supply-Demand Analysis
- 2.4. Competitive Benchmarking
- 2.5. Go-to- Market Strategy
- 2.5.1. Customer/ End-use Industry Assessment
- 2.5.2. Growth Opportunity Data, 2025-2035
- 2.5.2.1. Regional Data
- 2.5.2.2. Country Data
- 2.5.2.3. Segmental Data
- 2.5.3. Identification of Potential Market Spaces
- 2.5.4. GAP Analysis
- 2.5.5. Potential Attractive Price Points
- 2.5.6. Prevailing Market Risks & Challenges
- 2.5.7. Preferred Sales & Marketing Strategies
- 2.5.8. Key Recommendations and Analysis
- 2.5.9. A Way Forward
- 2.1. Global Healthcare Payer Technology and Services Market Outlook
- 3. Industry Data and Premium Insights
- 3.1. Global Healthcare & Pharmaceutical Industry Overview, 2025
- 3.1.1. Healthcare & Pharmaceutical Industry Ecosystem Analysis
- 3.1.2. Key Trends for Healthcare & Pharmaceutical Industry
- 3.1.3. Regional Distribution for Healthcare & Pharmaceutical Industry
- 3.2. Supplier Customer Data
- 3.3. Technology Roadmap and Developments
- 3.4. Trade Analysis
- 3.4.1. Import & Export Analysis, 2025
- 3.4.2. Top Importing Countries
- 3.4.3. Top Exporting Countries
- 3.5. Trump Tariff Impact Analysis
- 3.5.1. Manufacturer
- 3.5.1.1. Based on the component & Raw material
- 3.5.2. Supply Chain
- 3.5.3. End Consumer
- 3.5.1. Manufacturer
- 3.6. Raw Material Analysis
- 3.1. Global Healthcare & Pharmaceutical Industry Overview, 2025
- 4. Market Overview
- 4.1. Market Dynamics
- 4.1.1. Drivers
- 4.1.1.1. Value-based care & cost-containment pressures driving payer tech adoption
- 4.1.1.2. Advanced analytics/AI for risk stratification, personalization, and fraud detection
- 4.1.1.3. Regulatory mandates and interoperability pushing digital modernization
- 4.1.2. Restraints
- 4.1.2.1. Data privacy, security, and integration challenges
- 4.1.2.2. High implementation costs and legacy-system inertia
- 4.1.1. Drivers
- 4.2. Key Trend Analysis
- 4.3. Regulatory Framework
- 4.3.1. Key Regulations, Norms, and Subsidies, by Key Countries
- 4.3.2. Tariffs and Standards
- 4.3.3. Impact Analysis of Regulations on the Market
- 4.4. Value Chain Analysis
- 4.5. Porter’s Five Forces Analysis
- 4.6. PESTEL Analysis
- 4.7. Global Healthcare Payer Technology and Services Market Demand
- 4.7.1. Historical Market Size - in Value (US$ Bn), 2020-2024
- 4.7.2. Current and Future Market Size - in Value (US$ Bn), 2025–2035
- 4.7.2.1. Y-o-Y Growth Trends
- 4.7.2.2. Absolute $ Opportunity Assessment
- 4.1. Market Dynamics
- 5. Competition Landscape
- 5.1. Competition structure
- 5.1.1. Fragmented v/s consolidated
- 5.2. Company Share Analysis, 2025
- 5.2.1. Global Company Market Share
- 5.2.2. By Region
- 5.2.2.1. North America
- 5.2.2.2. Europe
- 5.2.2.3. Asia Pacific
- 5.2.2.4. Middle East
- 5.2.2.5. Africa
- 5.2.2.6. South America
- 5.3. Product Comparison Matrix
- 5.3.1. Specifications
- 5.3.2. Market Positioning
- 5.3.3. Pricing
- 5.1. Competition structure
- 6. Global Healthcare Payer Technology and Services Market Analysis, By Component
- 6.1. Key Segment Analysis
- 6.2. Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, By Component, 2021-2035
- 6.2.1. Software Solutions
- 6.2.1.1. Claims Management Software
- 6.2.1.2. Provider Network Management Software
- 6.2.1.3. Payment Integrity Software
- 6.2.1.4. Care Management Software
- 6.2.1.5. Member Management Software
- 6.2.1.6. Fraud, Waste, and Abuse Detection Software
- 6.2.1.7. Analytics and Reporting Software
- 6.2.1.8. Others
- 6.2.2. Services
- 6.2.2.1. Implementation Services
- 6.2.2.2. Consulting Services
- 6.2.2.3. Training and Education Services
- 6.2.2.4. Support and Maintenance Services
- 6.2.2.5. Managed Services
- 6.2.2.6. Others
- 6.2.1. Software Solutions
- 7. Global Healthcare Payer Technology and Services Market Analysis, By Deployment Mode
- 7.1. Key Segment Analysis
- 7.2. Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, By Deployment Mode, 2021-2035
- 7.2.1. On-Premises
- 7.2.2. Cloud-Based
- 7.2.3. Hosted Solutions
- 8. Global Healthcare Payer Technology and Services Market Analysis and Forecasts,By Payer Type
- 8.1. Key Findings
- 8.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Payer Type, 2021-2035
- 8.2.1. Private Payers
- 8.2.1.1. Commercial Health Insurance Companies
- 8.2.1.2. Managed Care Organizations (MCOs)
- 8.2.1.3. Third-Party Administrators (TPAs)
- 8.2.1.4. Others
- 8.2.2. Public Payers
- 8.2.2.1. Medicare Programs
- 8.2.2.2. Medicaid Programs
- 8.2.2.3. Government Health Agencies
- 8.2.2.4. Others
- 8.2.3. Hybrid Payers
- 8.2.1. Private Payers
- 9. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Organization Size
- 9.1. Key Findings
- 9.2. Healthcare Payer Technology and Services Market Size (Vo Value - US$ Mn), Analysis, and Forecasts, By Organization Size, 2021-2035
- 9.2.1. Large Enterprises
- 9.2.2. Small and Medium-sized Enterprises (SMEs)
- 10. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Service Model
- 10.1. Key Findings
- 10.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Service Model, 2021-2035
- 10.2.1. Business Process Outsourcing (BPO)
- 10.2.2. Knowledge Process Outsourcing (KPO)
- 10.2.3. Information Technology Outsourcing (ITO)
- 10.2.4. In-House Solutions
- 11. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Pricing Model
- 11.1. Key Findings
- 11.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Pricing Model, 2021-2035
- 11.2.1. Subscription-Based
- 11.2.2. Perpetual License
- 11.2.3. Pay-Per-Use
- 11.2.4. Transaction-Based
- 12. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By Integration Level
- 12.1. Key Findings
- 12.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By Integration Level, 2021-2035
- 12.2.1. Standalone Solutions
- 12.2.2. Integrated Platforms
- 12.2.3. Enterprise-Wide Systems
- 12.2.4. Interoperable Systems
- 13. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, By End-users
- 13.1. Key Findings
- 13.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, By End-users, 2021-2035
- 13.2.1. Health Insurance Companies
- 13.2.1.1. Member Enrollment and Eligibility Verification
- 13.2.1.2. Premium Billing and Collection
- 13.2.1.3. Claims Adjudication and Processing
- 13.2.1.4. Provider Credentialing and Network Management
- 13.2.1.5. Utilization Management
- 13.2.1.6. Risk Assessment and Underwriting
- 13.2.1.7. Customer Service and Support
- 13.2.1.8. Fraud Detection and Prevention
- 13.2.1.9. Others
- 13.2.2. Managed Care Organizations (MCOs)
- 13.2.2.1. Care Coordination and Management
- 13.2.2.2. Disease Management Programs
- 13.2.2.3. Population Health Management
- 13.2.2.4. Member Engagement Platforms
- 13.2.2.5. Pharmacy Benefit Management
- 13.2.2.6. Value-Based Care Analytics
- 13.2.2.7. Others
- 13.2.3. Third-Party Administrators (TPAs)
- 13.2.3.1. Claims Processing and Administration
- 13.2.3.2. Benefits Administration
- 13.2.3.3. COBRA Administration
- 13.2.3.4. Health Savings Account (HSA) Management
- 13.2.3.5. Flexible Spending Account (FSA) Administration
- 13.2.3.6. Provider Payment Processing
- 13.2.3.7. Others
- 13.2.4. Government Health Programs
- 13.2.4.1. Medicare/Medicaid Claims Processing
- 13.2.4.2. Eligibility Determination Systems
- 13.2.4.3. Program Integrity and Audit
- 13.2.4.4. Appeals and Grievance Management
- 13.2.4.5. Public Health Reporting
- 13.2.4.6. Others
- 13.2.5. Self-Insured Employers
- 13.2.5.1. Employee Benefits Administration
- 13.2.5.2. Health Plan Management
- 13.2.5.3. Wellness Program Management
- 13.2.5.4. Claims Analytics and Reporting
- 13.2.5.5. Cost Containment Strategies
- 13.2.5.6. Employee Health Data Analytics
- 13.2.5.7. Others
- 13.2.6. Pharmacy Benefit Managers (PBMs)
- 13.2.7. Healthcare Provider Organizations
- 13.2.8. Health and Wellness Companies
- 13.2.9. Other End-users
- 13.2.1. Health Insurance Companies
- 14. Global Healthcare Payer Technology and Services Market Analysis and Forecasts, by Region
- 14.1. Key Findings
- 14.2. Healthcare Payer Technology and Services Market Size (Value - US$ Mn), Analysis, and Forecasts, by Region, 2021-2035
- 14.2.1. North America
- 14.2.2. Europe
- 14.2.3. Asia Pacific
- 14.2.4. Middle East
- 14.2.5. Africa
- 14.2.6. South America
- 15. North America Healthcare Payer Technology and Services Market Analysis
- 15.1. Key Segment Analysis
- 15.2. Regional Snapshot
- 15.3. North America Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 15.3.1. Component
- 15.3.2. Deployment Mode
- 15.3.3. Payer Type
- 15.3.4. Organization Size
- 15.3.5. Service Model
- 15.3.6. Pricing Model
- 15.3.7. Integration Level
- 15.3.8. End-Users
- 15.3.9. Country
- 15.3.9.1. USA
- 15.3.9.2. Canada
- 15.3.9.3. Mexico
- 15.4. USA Healthcare Payer Technology and Services Market
- 15.4.1. Country Segmental Analysis
- 15.4.2. Component
- 15.4.3. Deployment Mode
- 15.4.4. Payer Type
- 15.4.5. Organization Size
- 15.4.6. Service Model
- 15.4.7. Pricing Model
- 15.4.8. Integration Level
- 15.4.9. End-Users
- 15.5. Canada Healthcare Payer Technology and Services Market
- 15.5.1. Country Segmental Analysis
- 15.5.2. Component
- 15.5.3. Deployment Mode
- 15.5.4. Payer Type
- 15.5.5. Organization Size
- 15.5.6. Service Model
- 15.5.7. Pricing Model
- 15.5.8. Integration Level
- 15.5.9. End-Users
- 15.6. Mexico Healthcare Payer Technology and Services Market
- 15.6.1. Country Segmental Analysis
- 15.6.2. Component
- 15.6.3. Deployment Mode
- 15.6.4. Payer Type
- 15.6.5. Organization Size
- 15.6.6. Service Model
- 15.6.7. Pricing Model
- 15.6.8. Integration Level
- 15.6.9. End-Users
- 16. Europe Healthcare Payer Technology and Services Market Analysis
- 16.1. Key Segment Analysis
- 16.2. Regional Snapshot
- 16.3. Europe Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 16.3.1. Component
- 16.3.2. Deployment Mode
- 16.3.3. Payer Type
- 16.3.4. Organization Size
- 16.3.5. Service Model
- 16.3.6. Pricing Model
- 16.3.7. Integration Level
- 16.3.8. End-Users
- 16.3.9. Country
- 16.3.9.1. Germany
- 16.3.9.2. United Kingdom
- 16.3.9.3. France
- 16.3.9.4. Italy
- 16.3.9.5. Spain
- 16.3.9.6. Netherlands
- 16.3.9.7. Nordic Countries
- 16.3.9.8. Poland
- 16.3.9.9. Russia & CIS
- 16.3.9.10. Rest of Europe
- 16.4. Germany Healthcare Payer Technology and Services Market
- 16.4.1. Country Segmental Analysis
- 16.4.2. Component
- 16.4.3. Deployment Mode
- 16.4.4. Payer Type
- 16.4.5. Organization Size
- 16.4.6. Service Model
- 16.4.7. Pricing Model
- 16.4.8. Integration Level
- 16.4.9. End-Users
- 16.5. United Kingdom Healthcare Payer Technology and Services Market
- 16.5.1. Country Segmental Analysis
- 16.5.2. Component
- 16.5.3. Deployment Mode
- 16.5.4. Payer Type
- 16.5.5. Organization Size
- 16.5.6. Service Model
- 16.5.7. Pricing Model
- 16.5.8. Integration Level
- 16.5.9. End-Users
- 16.6. France Healthcare Payer Technology and Services Market
- 16.6.1. Country Segmental Analysis
- 16.6.2. Component
- 16.6.3. Deployment Mode
- 16.6.4. Payer Type
- 16.6.5. Organization Size
- 16.6.6. Service Model
- 16.6.7. Pricing Model
- 16.6.8. Integration Level
- 16.6.9. End-Users
- 16.7. Italy Healthcare Payer Technology and Services Market
- 16.7.1. Country Segmental Analysis
- 16.7.2. Component
- 16.7.3. Deployment Mode
- 16.7.4. Payer Type
- 16.7.5. Organization Size
- 16.7.6. Service Model
- 16.7.7. Pricing Model
- 16.7.8. Integration Level
- 16.7.9. End-Users
- 16.8. Spain Healthcare Payer Technology and Services Market
- 16.8.1. Component
- 16.8.2. Deployment Mode
- 16.8.3. Payer Type
- 16.8.4. Organization Size
- 16.8.5. Service Model
- 16.8.6. Pricing Model
- 16.8.7. Integration Level
- 16.8.8. End-Users
- 16.9. Netherlands Healthcare Payer Technology and Services Market
- 16.9.1. Country Segmental Analysis
- 16.9.2. Component
- 16.9.3. Deployment Mode
- 16.9.4. Payer Type
- 16.9.5. Organization Size
- 16.9.6. Service Model
- 16.9.7. Pricing Model
- 16.9.8. Integration Level
- 16.9.9. End-Users
- 16.10. Nordic Countries Healthcare Payer Technology and Services Market
- 16.10.1. Country Segmental Analysis
- 16.10.2. Component
- 16.10.3. Deployment Mode
- 16.10.4. Payer Type
- 16.10.5. Organization Size
- 16.10.6. Service Model
- 16.10.7. Pricing Model
- 16.10.8. Integration Level
- 16.10.9. End-Users
- 16.11. Poland Healthcare Payer Technology and Services Market
- 16.11.1. Country Segmental Analysis
- 16.11.2. Component
- 16.11.3. Deployment Mode
- 16.11.4. Payer Type
- 16.11.5. Organization Size
- 16.11.6. Service Model
- 16.11.7. Pricing Model
- 16.11.8. Integration Level
- 16.11.9. End-Users
- 16.12. Russia & CIS Healthcare Payer Technology and Services Market
- 16.12.1. Country Segmental Analysis
- 16.12.2. Component
- 16.12.3. Deployment Mode
- 16.12.4. Payer Type
- 16.12.5. Organization Size
- 16.12.6. Service Model
- 16.12.7. Pricing Model
- 16.12.8. Integration Level
- 16.12.9. End-Users
- 16.13. Rest of Europe Healthcare Payer Technology and Services Market
- 16.13.1. Country Segmental Analysis
- 16.13.2. Component
- 16.13.3. Deployment Mode
- 16.13.4. Payer Type
- 16.13.5. Organization Size
- 16.13.6. Service Model
- 16.13.7. Pricing Model
- 16.13.8. Integration Level
- 16.13.9. End-Users
- 17. Asia Pacific Healthcare Payer Technology and Services Market Analysis
- 17.1. Key Segment Analysis
- 17.2. Regional Snapshot
- 17.3. East Asia Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 17.3.1. Component
- 17.3.2. Deployment Mode
- 17.3.3. Payer Type
- 17.3.4. Organization Size
- 17.3.5. Service Model
- 17.3.6. Pricing Model
- 17.3.7. Integration Level
- 17.3.8. End-Users
- 17.3.9. Country
- 17.3.9.1. China
- 17.3.9.2. India
- 17.3.9.3. Japan
- 17.3.9.4. South Korea
- 17.3.9.5. Australia and New Zealand
- 17.3.9.6. Indonesia
- 17.3.9.7. Malaysia
- 17.3.9.8. Thailand
- 17.3.9.9. Vietnam
- 17.3.9.10. Rest of Asia Pacific
- 17.4. China Healthcare Payer Technology and Services Market
- 17.4.1. Country Segmental Analysis
- 17.4.2. Component
- 17.4.3. Deployment Mode
- 17.4.4. Payer Type
- 17.4.5. Organization Size
- 17.4.6. Service Model
- 17.4.7. Pricing Model
- 17.4.8. Integration Level
- 17.4.9. End-Users
- 17.5. India Healthcare Payer Technology and Services Market
- 17.5.1. Country Segmental Analysis
- 17.5.2. Component
- 17.5.3. Deployment Mode
- 17.5.4. Payer Type
- 17.5.5. Organization Size
- 17.5.6. Service Model
- 17.5.7. Pricing Model
- 17.5.8. Integration Level
- 17.5.9. End-Users
- 17.6. Japan Healthcare Payer Technology and Services Market
- 17.6.1. Country Segmental Analysis
- 17.6.2. Component
- 17.6.3. Deployment Mode
- 17.6.4. Payer Type
- 17.6.5. Organization Size
- 17.6.6. Service Model
- 17.6.7. Pricing Model
- 17.6.8. Integration Level
- 17.6.9. End-Users
- 17.7. South Korea Healthcare Payer Technology and Services Market
- 17.7.1. Country Segmental Analysis
- 17.7.2. Component
- 17.7.3. Deployment Mode
- 17.7.4. Payer Type
- 17.7.5. Organization Size
- 17.7.6. Service Model
- 17.7.7. Pricing Model
- 17.7.8. Integration Level
- 17.7.9. End-Users
- 17.8. Australia and New Zealand Healthcare Payer Technology and Services Market
- 17.8.1. Country Segmental Analysis
- 17.8.2. Component
- 17.8.3. Deployment Mode
- 17.8.4. Payer Type
- 17.8.5. Organization Size
- 17.8.6. Service Model
- 17.8.7. Pricing Model
- 17.8.8. Integration Level
- 17.8.9. End-Users
- 17.9. Indonesia Healthcare Payer Technology and Services Market
- 17.9.1. Country Segmental Analysis
- 17.9.2. Component
- 17.9.3. Deployment Mode
- 17.9.4. Payer Type
- 17.9.5. Organization Size
- 17.9.6. Service Model
- 17.9.7. Pricing Model
- 17.9.8. Integration Level
- 17.9.9. End-Users
- 17.10. Malaysia Healthcare Payer Technology and Services Market
- 17.10.1. Country Segmental Analysis
- 17.10.2. Component
- 17.10.3. Deployment Mode
- 17.10.4. Payer Type
- 17.10.5. Organization Size
- 17.10.6. Service Model
- 17.10.7. Pricing Model
- 17.10.8. Integration Level
- 17.10.9. End-Users
- 17.11. Thailand Healthcare Payer Technology and Services Market
- 17.11.1. Country Segmental Analysis
- 17.11.2. Component
- 17.11.3. Deployment Mode
- 17.11.4. Payer Type
- 17.11.5. Organization Size
- 17.11.6. Service Model
- 17.11.7. Pricing Model
- 17.11.8. Integration Level
- 17.11.9. End-Users
- 17.12. Vietnam Healthcare Payer Technology and Services Market
- 17.12.1. Country Segmental Analysis
- 17.12.2. Component
- 17.12.3. Deployment Mode
- 17.12.4. Payer Type
- 17.12.5. Organization Size
- 17.12.6. Service Model
- 17.12.7. Pricing Model
- 17.12.8. Integration Level
- 17.12.9. End-Users
- 17.13. Rest of Asia Pacific Healthcare Payer Technology and Services Market
- 17.13.1. Country Segmental Analysis
- 17.13.2. Component
- 17.13.3. Deployment Mode
- 17.13.4. Payer Type
- 17.13.5. Organization Size
- 17.13.6. Service Model
- 17.13.7. Pricing Model
- 17.13.8. Integration Level
- 17.13.9. End-Users
- 18. Middle East Healthcare Payer Technology and Services Market Analysis
- 18.1. Key Segment Analysis
- 18.2. Regional Snapshot
- 18.3. Middle East Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 18.3.1. Component
- 18.3.2. Deployment Mode
- 18.3.3. Payer Type
- 18.3.4. Organization Size
- 18.3.5. Service Model
- 18.3.6. Pricing Model
- 18.3.7. Integration Level
- 18.3.8. End-Users
- 18.3.9. Country
- 18.3.9.1. Turkey
- 18.3.9.2. UAE
- 18.3.9.3. Saudi Arabia
- 18.3.9.4. Israel
- 18.3.9.5. Rest of Middle East
- 18.4. Turkey Healthcare Payer Technology and Services Market
- 18.4.1. Country Segmental Analysis
- 18.4.2. Component
- 18.4.3. Deployment Mode
- 18.4.4. Payer Type
- 18.4.5. Organization Size
- 18.4.6. Service Model
- 18.4.7. Pricing Model
- 18.4.8. Integration Level
- 18.4.9. End-Users
- 18.5. UAE Healthcare Payer Technology and Services Market
- 18.5.1. Country Segmental Analysis
- 18.5.2. Component
- 18.5.3. Deployment Mode
- 18.5.4. Payer Type
- 18.5.5. Organization Size
- 18.5.6. Service Model
- 18.5.7. Pricing Model
- 18.5.8. Integration Level
- 18.5.9. End-Users
- 18.6. Saudi Arabia Healthcare Payer Technology and Services Market
- 18.6.1. Country Segmental Analysis
- 18.6.2. Component
- 18.6.3. Deployment Mode
- 18.6.4. Payer Type
- 18.6.5. Organization Size
- 18.6.6. Service Model
- 18.6.7. Pricing Model
- 18.6.8. Integration Level
- 18.6.9. End-Users
- 18.7. Israel Healthcare Payer Technology and Services Market
- 18.7.1. Country Segmental Analysis
- 18.7.2. Component
- 18.7.3. Deployment Mode
- 18.7.4. Payer Type
- 18.7.5. Organization Size
- 18.7.6. Service Model
- 18.7.7. Pricing Model
- 18.7.8. Integration Level
- 18.7.9. End-Users
- 18.8. Rest of Middle East Healthcare Payer Technology and Services Market
- 18.8.1. Country Segmental Analysis
- 18.8.2. Component
- 18.8.3. Deployment Mode
- 18.8.4. Payer Type
- 18.8.5. Organization Size
- 18.8.6. Service Model
- 18.8.7. Pricing Model
- 18.8.8. Integration Level
- 18.8.9. End-Users
- 19. Africa Healthcare Payer Technology and Services Market Analysis
- 19.1. Key Segment Analysis
- 19.2. Regional Snapshot
- 19.3. Africa Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 19.3.1. Component
- 19.3.2. Deployment Mode
- 19.3.3. Payer Type
- 19.3.4. Organization Size
- 19.3.5. Service Model
- 19.3.6. Pricing Model
- 19.3.7. Integration Level
- 19.3.8. End-Users
- 19.3.9. Country
- 19.3.9.1. South Africa
- 19.3.9.2. Egypt
- 19.3.9.3. Nigeria
- 19.3.9.4. Algeria
- 19.3.9.5. Rest of Africa
- 19.4. South Africa Healthcare Payer Technology and Services Market
- 19.4.1. Country Segmental Analysis
- 19.4.2. Component
- 19.4.3. Deployment Mode
- 19.4.4. Payer Type
- 19.4.5. Organization Size
- 19.4.6. Service Model
- 19.4.7. Pricing Model
- 19.4.8. Integration Level
- 19.4.9. End-Users
- 19.5. Egypt Healthcare Payer Technology and Services Market
- 19.5.1. Country Segmental Analysis
- 19.5.2. Component
- 19.5.3. Deployment Mode
- 19.5.4. Payer Type
- 19.5.5. Organization Size
- 19.5.6. Service Model
- 19.5.7. Pricing Model
- 19.5.8. Integration Level
- 19.5.9. End-Users
- 19.6. Nigeria Healthcare Payer Technology and Services Market
- 19.6.1. Country Segmental Analysis
- 19.6.2. Component
- 19.6.3. Deployment Mode
- 19.6.4. Payer Type
- 19.6.5. Organization Size
- 19.6.6. Service Model
- 19.6.7. Pricing Model
- 19.6.8. Integration Level
- 19.6.9. End-Users
- 19.7. Algeria Healthcare Payer Technology and Services Market
- 19.7.1. Country Segmental Analysis
- 19.7.2. Component
- 19.7.3. Deployment Mode
- 19.7.4. Payer Type
- 19.7.5. Organization Size
- 19.7.6. Service Model
- 19.7.7. Pricing Model
- 19.7.8. Integration Level
- 19.7.9. End-Users
- 19.8. Rest of Africa Healthcare Payer Technology and Services Market
- 19.8.1. Country Segmental Analysis
- 19.8.2. Component
- 19.8.3. Deployment Mode
- 19.8.4. Payer Type
- 19.8.5. Organization Size
- 19.8.6. Service Model
- 19.8.7. Pricing Model
- 19.8.8. Integration Level
- 19.8.9. End-Users
- 20. South America Healthcare Payer Technology and Services Market Analysis
- 20.1. Key Segment Analysis
- 20.2. Regional Snapshot
- 20.3. Central and South Africa Healthcare Payer Technology and Services Market Size (Value - US$ Bn), Analysis, and Forecasts, 2021-2035
- 20.3.1. Component
- 20.3.2. Deployment Mode
- 20.3.3. Payer Type
- 20.3.4. Organization Size
- 20.3.5. Service Model
- 20.3.6. Pricing Model
- 20.3.7. Integration Level
- 20.3.8. End-Users
- 20.3.9. Country
- 20.3.9.1. Brazil
- 20.3.9.2. Argentina
- 20.3.9.3. Rest of South America
- 20.4. Brazil Healthcare Payer Technology and Services Market
- 20.4.1. Country Segmental Analysis
- 20.4.2. Component
- 20.4.3. Deployment Mode
- 20.4.4. Payer Type
- 20.4.5. Organization Size
- 20.4.6. Service Model
- 20.4.7. Pricing Model
- 20.4.8. Integration Level
- 20.4.9. End-Users
- 20.5. Argentina Healthcare Payer Technology and Services Market
- 20.5.1. Country Segmental Analysis
- 20.5.2. Component
- 20.5.3. Deployment Mode
- 20.5.4. Payer Type
- 20.5.5. Organization Size
- 20.5.6. Service Model
- 20.5.7. Pricing Model
- 20.5.8. Integration Level
- 20.5.9. End-Users
- 20.6. Rest of South America Healthcare Payer Technology and Services Market
- 20.6.1. Country Segmental Analysis
- 20.6.2. Component
- 20.6.3. Deployment Mode
- 20.6.4. Payer Type
- 20.6.5. Organization Size
- 20.6.6. Service Model
- 20.6.7. Pricing Model
- 20.6.8. Integration Level
- 20.6.9. End-Users
- 21. Key Players/ Company Profile
- 21.1. Accenture
- 21.1.1. Company Details/ Overview
- 21.1.2. Company Financials
- 21.1.3. Key Customers and Competitors
- 21.1.4. Business/ Industry Portfolio
- 21.1.5. Product Portfolio/ Specification Details
- 21.1.6. Pricing Data
- 21.1.7. Strategic Overview
- 21.1.8. Recent Developments
- 21.2. Allscripts Healthcare Solutions
- 21.3. Atos SE
- 21.4. CGI Inc.
- 21.5. Cognizant Technology Solutions
- 21.6. Conduent Inc.
- 21.7. Conifer Health Solutions
- 21.8. DXC Technology
- 21.9. Evolent Health
- 21.10. EXL Service Holdings
- 21.11. Genpact
- 21.12. HCL Technologies
- 21.13. Hinduja Global Solutions (HGS)
- 21.14. IBM Corporation
- 21.15. Infosys
- 21.16. Inovalon Holdings
- 21.17. NTT DATA Corporation
- 21.18. Tata Consultancy Services (TCS)
- 21.19. TriZetto Corporation
- 21.20. UnitedHealth Group (Optum)
- 21.21. Wipro Limited
- 21.22. Other Key Players
- 21.1. Accenture
Note* - This is just tentative list of players. While providing the report, we will cover more number of players based on their revenue and share for each geography
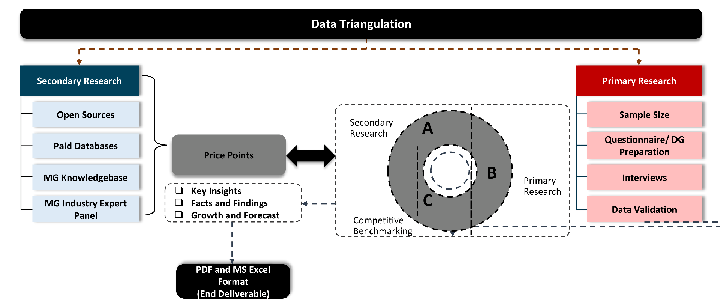
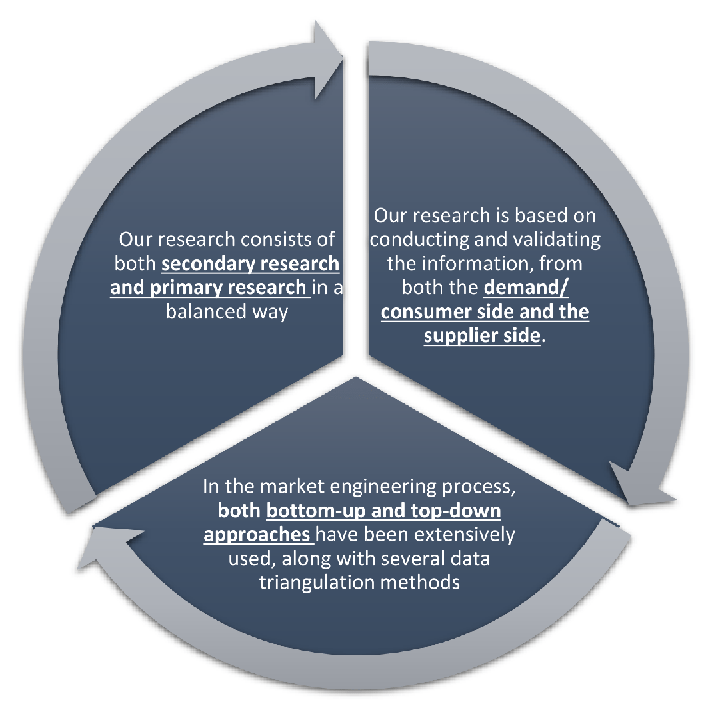
Our research design integrates both demand-side and supply-side analysis through a balanced combination of primary and secondary research methodologies. By utilizing both bottom-up and top-down approaches alongside rigorous data triangulation methods, we deliver robust market intelligence that supports strategic decision-making.
MarketGenics' comprehensive research design framework ensures the delivery of accurate, reliable, and actionable market intelligence. Through the integration of multiple research approaches, rigorous validation processes, and expert analysis, we provide our clients with the insights needed to make informed strategic decisions and capitalize on market opportunities.
MarketGenics leverages a dedicated industry panel of experts and a comprehensive suite of paid databases to effectively collect, consolidate, and analyze market intelligence.
Our approach has consistently proven to be reliable and effective in generating accurate market insights, identifying key industry trends, and uncovering emerging business opportunities.
Through both primary and secondary research, we capture and analyze critical company-level data such as manufacturing footprints, including technical centers, R&D facilities, sales offices, and headquarters.
Our expert panel further enhances our ability to estimate market size for specific brands based on validated field-level intelligence.
Our data mining techniques incorporate both parametric and non-parametric methods, allowing for structured data collection, sorting, processing, and cleaning.
Demand projections are derived from large-scale data sets analyzed through proprietary algorithms, culminating in robust and reliable market sizing.
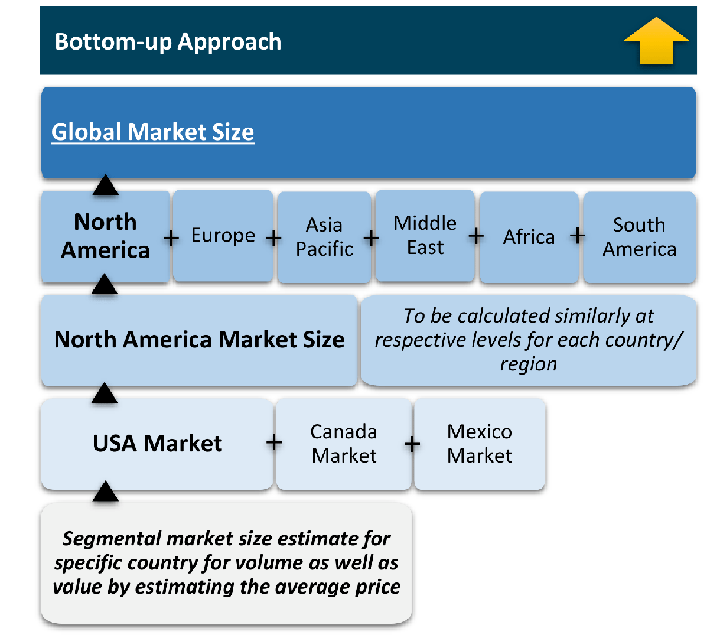
The bottom-up approach builds market estimates by starting with the smallest addressable market units and systematically aggregating them to create comprehensive market size projections.
This method begins with specific, granular data points and builds upward to create the complete market landscape.
Customer Analysis → Segmental Analysis → Geographical Analysis
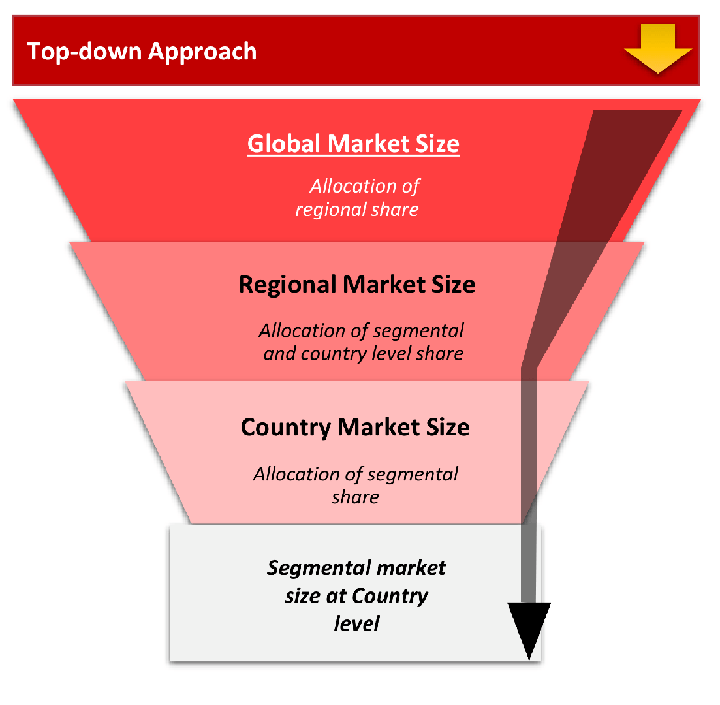
The top-down approach starts with the broadest possible market data and systematically narrows it down through a series of filters and assumptions to arrive at specific market segments or opportunities.
This method begins with the big picture and works downward to increasingly specific market slices.
TAM → SAM → SOM
While analysing the market, we extensively study secondary sources, directories, and databases to identify and collect information useful for this technical, market-oriented, and commercial report. Secondary sources that we utilize are not only the public sources, but it is combination of Open Source, Associations, Paid Databases, MG Repository & Knowledgebase and Others.
- Company websites, annual reports, financial reports, broker reports, and investor presentations
- National government documents, statistical databases and reports
- News articles, press releases and web-casts specific to the companies operating in the market, Magazines, reports, and others
- We gather information from commercial data sources for deriving company specific data such as segmental revenue, share for geography, product revenue, and others
- Internal and external proprietary databases (industry-specific), relevant patent, and regulatory databases
- Governing Bodies, Government Organizations
- Relevant Authorities, Country-specific Associations for Industries
We also employ the model mapping approach to estimate the product level market data through the players product portfolio
Primary research/ interviews is vital in analyzing the market. Most of the cases involves paid primary interviews. Primary sources includes primary interviews through e-mail interactions, telephonic interviews, surveys as well as face-to-face interviews with the different stakeholders across the value chain including several industry experts.
| Type of Respondents | Number of Primaries |
|---|---|
| Tier 2/3 Suppliers | ~20 |
| Tier 1 Suppliers | ~25 |
| End-users | ~25 |
| Industry Expert/ Panel/ Consultant | ~30 |
| Total | ~100 |
MG Knowledgebase
• Repository of industry blog, newsletter and case studies
• Online platform covering detailed market reports, and company profiles
- Historical Trends – Past market patterns, cycles, and major events that shaped how markets behave over time. Understanding past trends helps predict future behavior.
- Industry Factors – Specific characteristics of the industry like structure, regulations, and innovation cycles that affect market dynamics.
- Macroeconomic Factors – Economic conditions like GDP growth, inflation, and employment rates that affect how much money people have to spend.
- Demographic Factors – Population characteristics like age, income, and location that determine who can buy your product.
- Technology Factors – How quickly people adopt new technology and how much technology infrastructure exists.
- Regulatory Factors – Government rules, laws, and policies that can help or restrict market growth.
- Competitive Factors – Analyzing competition structure such as degree of competition and bargaining power of buyers and suppliers.
Multiple Regression Analysis
- Identify and quantify factors that drive market changes
- Statistical modeling to establish relationships between market drivers and outcomes
Time Series Analysis – Seasonal Patterns
- Understand regular cyclical patterns in market demand
- Advanced statistical techniques to separate trend, seasonal, and irregular components
Time Series Analysis – Trend Analysis
- Identify underlying market growth patterns and momentum
- Statistical analysis of historical data to project future trends
Expert Opinion – Expert Interviews
- Gather deep industry insights and contextual understanding
- In-depth interviews with key industry stakeholders
Multi-Scenario Development
- Prepare for uncertainty by modeling different possible futures
- Creating optimistic, pessimistic, and most likely scenarios
Time Series Analysis – Moving Averages
- Sophisticated forecasting for complex time series data
- Auto-regressive integrated moving average models with seasonal components
Econometric Models
- Apply economic theory to market forecasting
- Sophisticated economic models that account for market interactions
Expert Opinion – Delphi Method
- Harness collective wisdom of industry experts
- Structured, multi-round expert consultation process
Monte Carlo Simulation
- Quantify uncertainty and probability distributions
- Thousands of simulations with varying input parameters
Our research framework is built upon the fundamental principle of validating market intelligence from both demand and supply perspectives. This dual-sided approach ensures comprehensive market understanding and reduces the risk of single-source bias.
Demand-Side Analysis: We understand end-user/application behavior, preferences, and market needs along with the penetration of the product for specific application.
Supply-Side Analysis: We estimate overall market revenue, analyze the segmental share along with industry capacity, competitive landscape, and market structure.
Data triangulation is a validation technique that uses multiple methods, sources, or perspectives to examine the same research question, thereby increasing the credibility and reliability of research findings. In market research, triangulation serves as a quality assurance mechanism that helps identify and minimize bias, validate assumptions, and ensure accuracy in market estimates.
- Data Source Triangulation – Using multiple data sources to examine the same phenomenon
- Methodological Triangulation – Using multiple research methods to study the same research question
- Investigator Triangulation – Using multiple researchers or analysts to examine the same data
- Theoretical Triangulation – Using multiple theoretical perspectives to interpret the same data